Minimally Invasive Anterior Approach Total Hip Replacement
Home » Operations » Hip Surgery » Total Hip Replacement » Minimally Invasive Anterior Approach Total Hip Replacement
Related News:

The bikini incision: A new type of minimally invasive anterior approach in Total Hip Replacement
The “Bikini” incision is an evolution of Hueter’s minimally invasive anterior approach which allows to fit a total hip replacement while preserving the surrounding anatomical structures, ie without musculotendinous section, thus reducing the recovery time and the risk of dislocation of the prosthesis. It is simply a change in the position of the skin opening which, instead of being vertical in the axis of the thigh, occurs horizontally parallel to the skin folds.
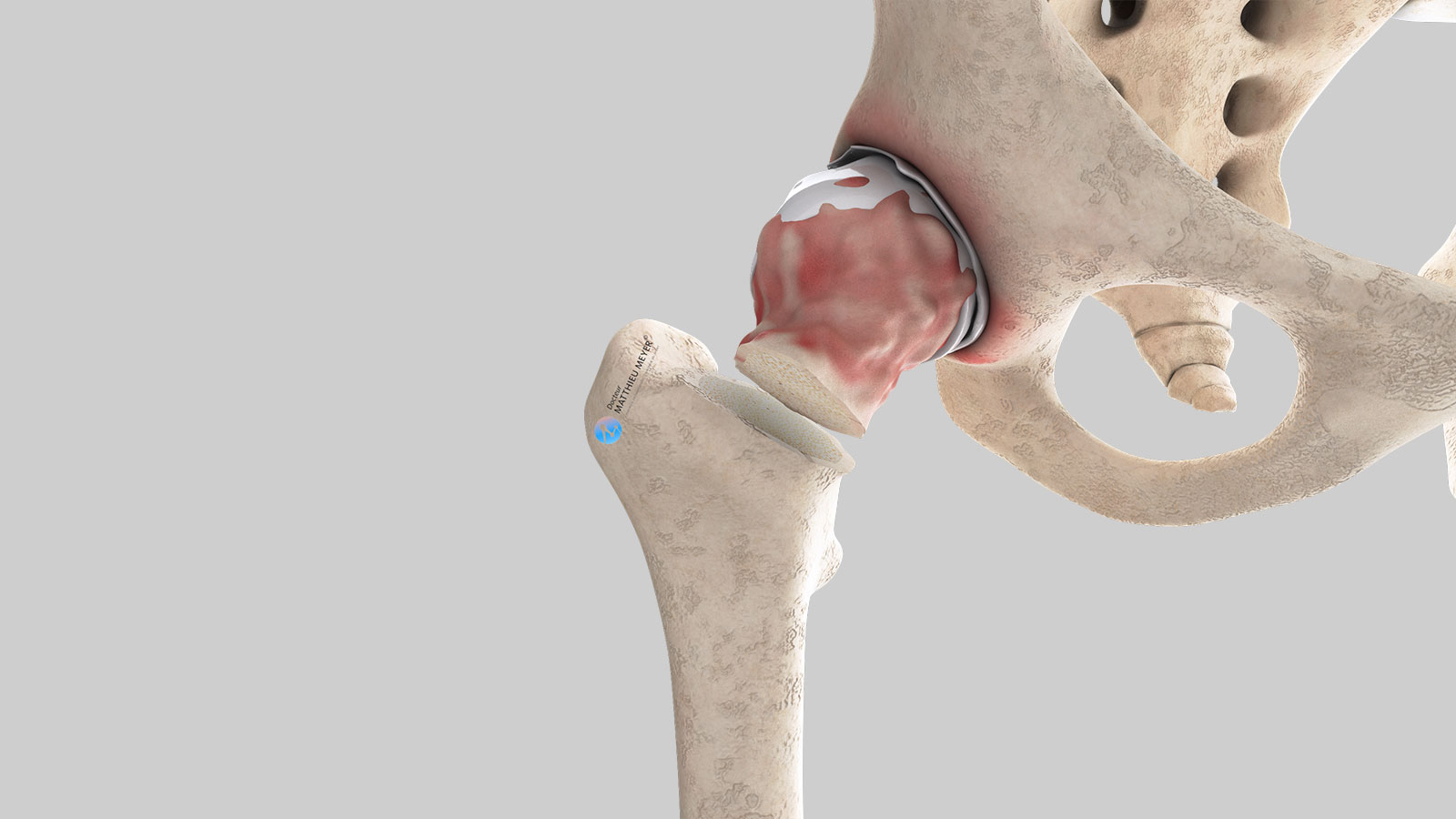
What is the problem?
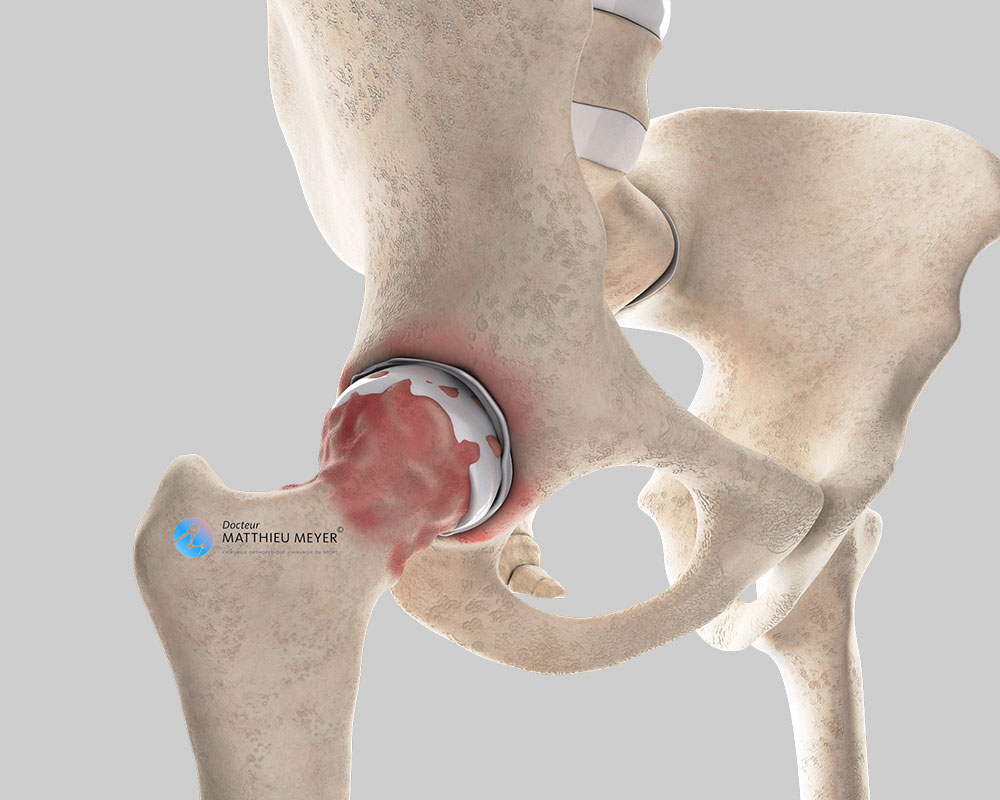
The hip is the joint between the pelvis and the femur, and like all joints, is covered with cartilage, a smooth substance with no nerve endings enabling the joint to move freely and painlessly. This cartilage can deteriorate for various reasons, especially in the case of hip osteoarthritis or inflammatory rheumatism such as rheumatoid arthritis or ankylosing spondylitis resulting in exposure of the rough and innervated underlying bone. The joint gradually becomes stiff and painful. When medical treatments (analgesics or injections) are no longer enough to relieve the pain, a total hip replacement is necessary to replace the worn cartilage. A hip replacement may also be necessary in the case of aseptic osteonecrosis of the femoral head. This destroys and deforms the femoral head resulting in significant hip pain.
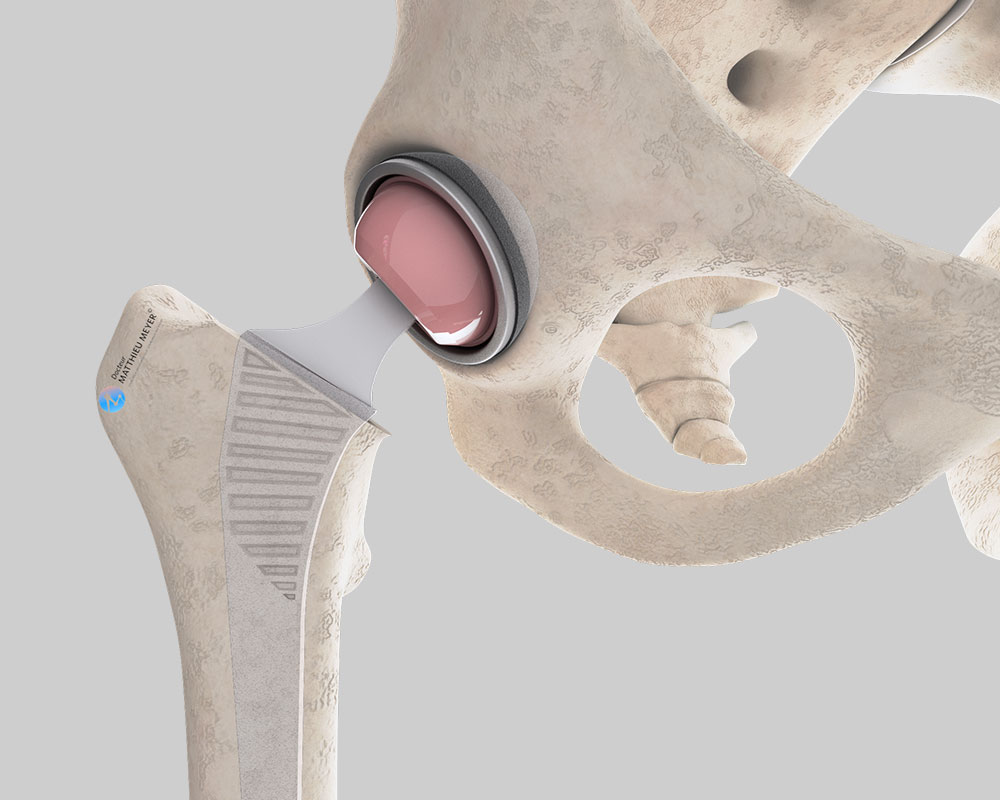
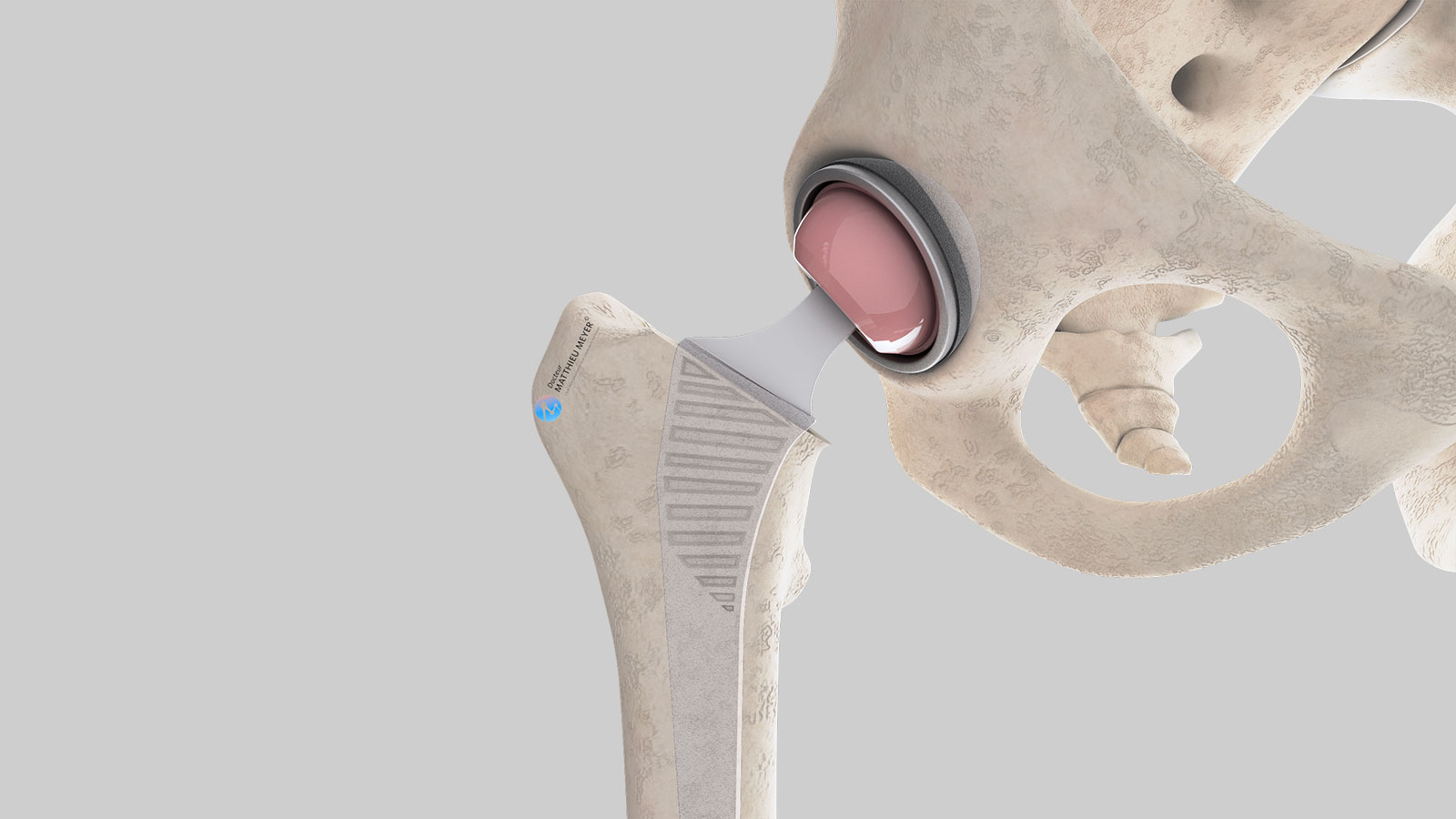
A total hip replacement replaces the cartilage of the pelvis and the femoral head and comprises two components called implants:
- An acetabular component attached to the pelvis
- A femoral stem attached to the femur
Before the operation
A total hip replacement requires an operation and the type of prosthesis best suited to the patient is chosen during the pre-surgical consultations. A pre-anaesthesia consultation and a preoperative assessment are also conducted before the operation to check the patient is physically apt to undergo the surgery and minimise the risk of postoperative complications, especially infections. This assessment generally includes a blood test, a cardiovascular check-up, as well as a dental check-up to ensure there are no infections and thus avoid any microbial contamination of the prosthesis.
Choice of prosthesis
The primary differences in the types of hip prostheses concern the following:
- The bearing surfaces
- The attachment to the bone
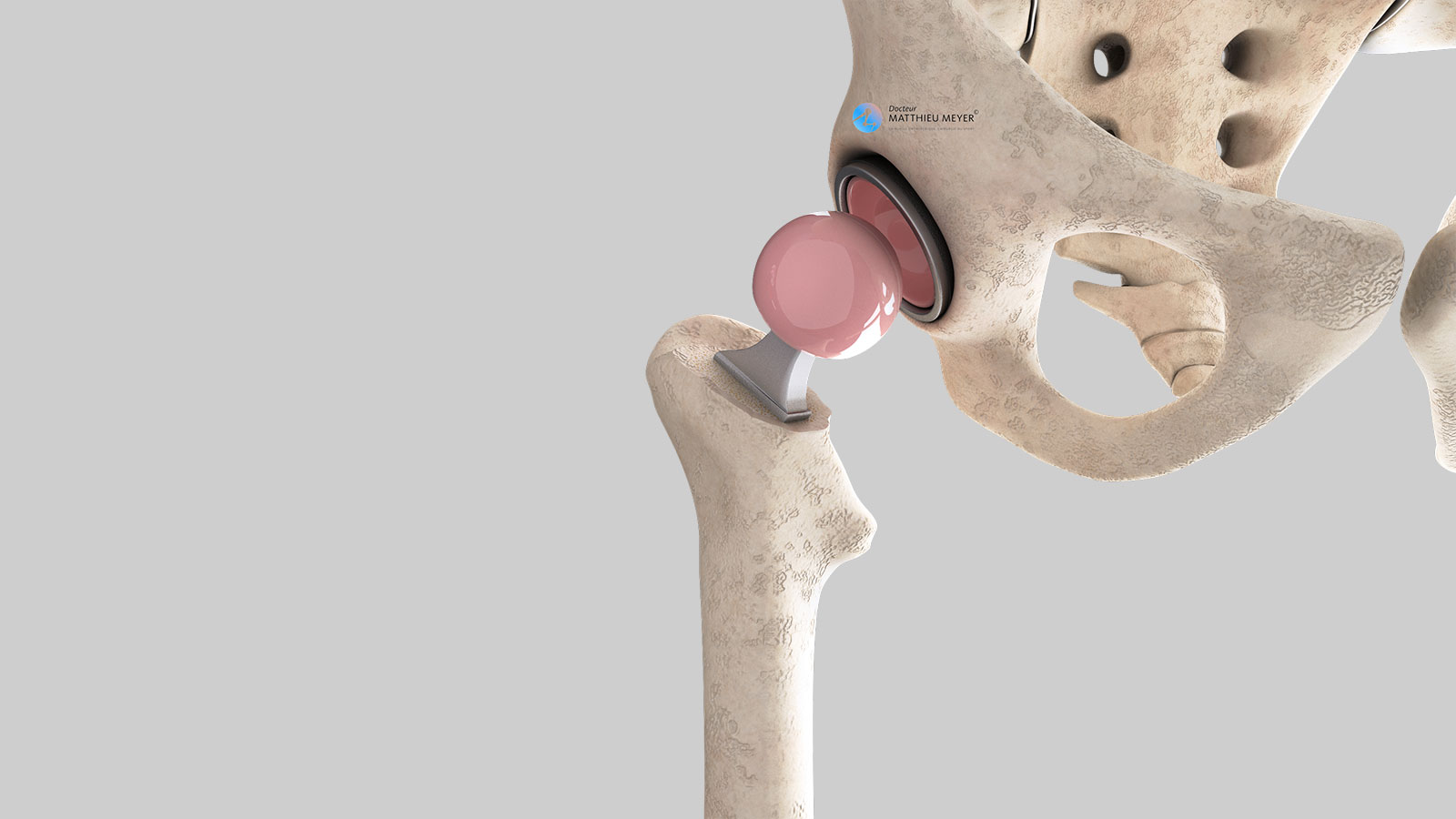
Bearing surfaces
This is the area where the two components of the implant are in contact and slide over each other thus ensuring joint mobility. The choice of materials of these bearing surfaces is fundamental as it has a direct impact on the lifespan of the implant. Ceramic bearing surfaces are currently preferred as there is practically zero wear. For the acetabular component, a highly reticulated very low-wear polyethene (plastic) surface is sometimes used.
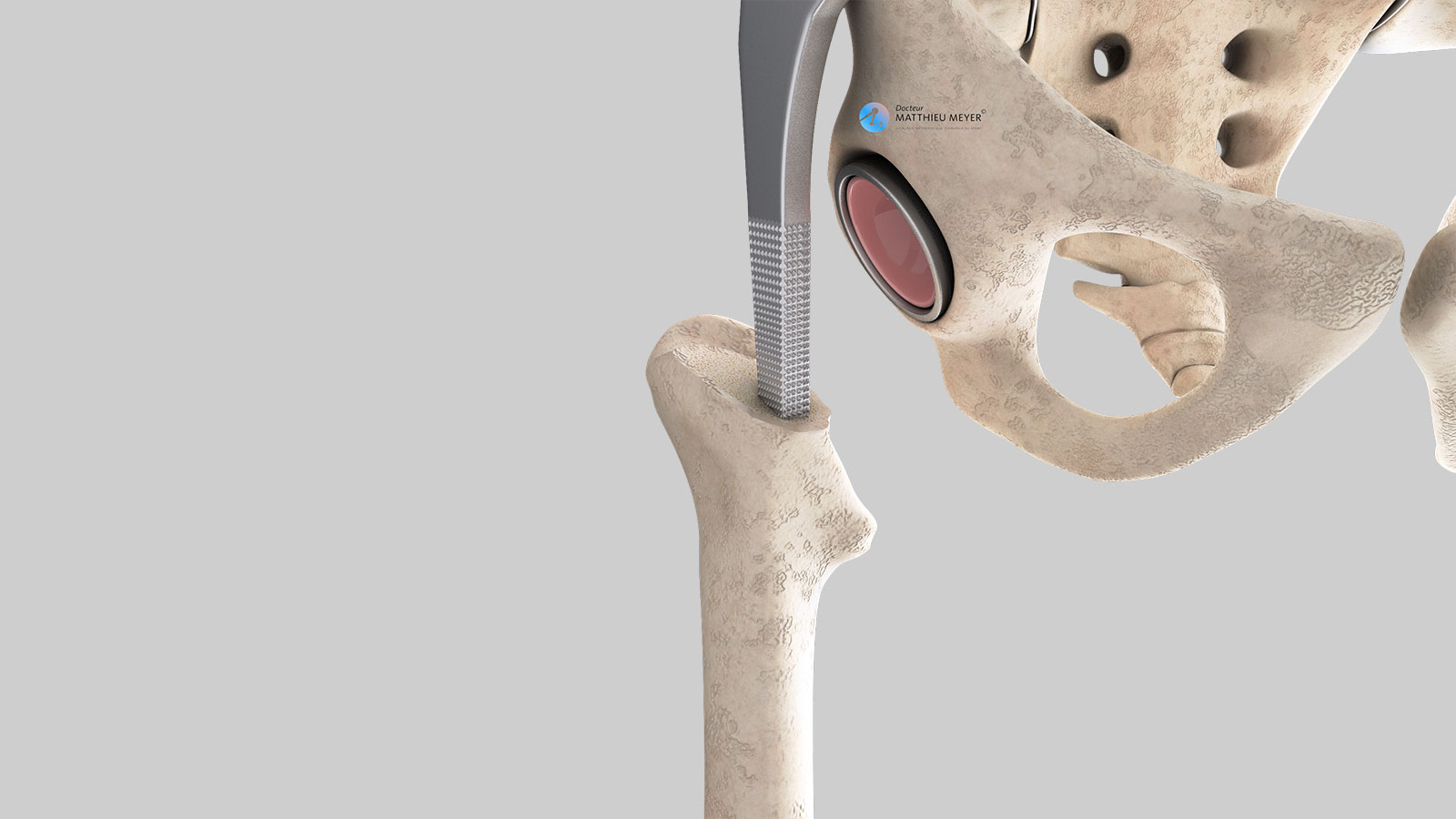
Fixation of the prosthesis
Fixation of the implant in the bone can be achieved in two ways. The implant can be cemented in the bone, in other words, a cement is poured into the bone in which the implant will be positioned and thus bond to the bone, or the surface of the implant can be textured (‘cementless’ fixation) and the bone in direct contact with the implant grows and secures it in place. The type of fixation depends on the quality of the bone, some anatomical factors, and the bearing surfaces chosen by the surgeon.
Size of the prosthesis
The sizes of the implants vary to match the anatomy of the patient undergoing the operation as closely as possible. Before the operation, the size of the prosthesis is determined using an x-ray or a scan. This step is fundamental, as it limits the risk of a length discrepancy of the lower limbs following the operation. CT-scan planning software is sometimes useful, especially for patients with an ‘unusually’ shaped hip for whom a customized femoral stem is sometimes used.
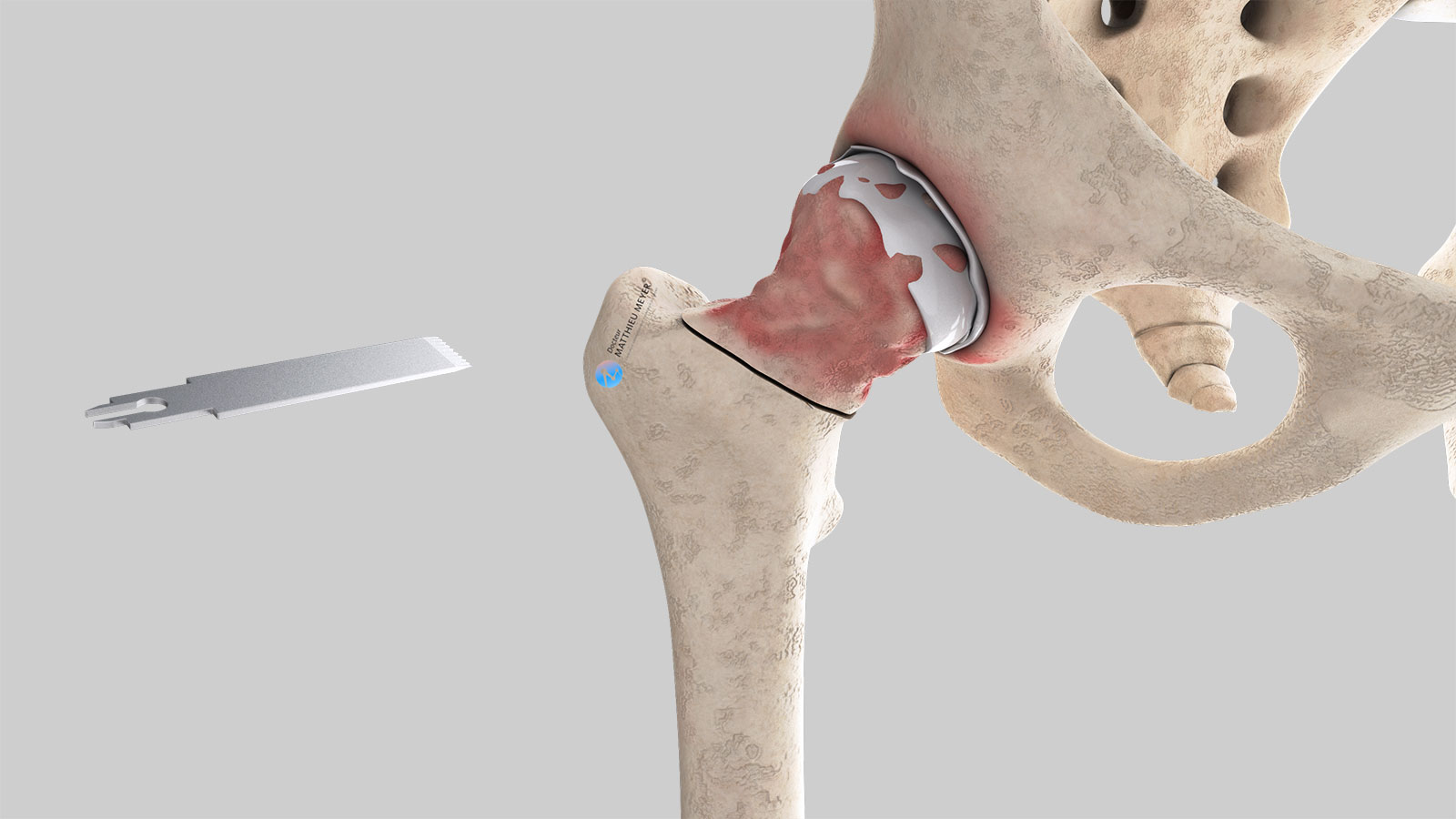
The operation
The operation takes place in an operating theatre in compliance with strict standards of cleanliness and safety. The patient is placed supine on the operating table.
The operation lasts about 1 hour, plus the time required for the anaesthetic and positioning the patient on the operating table. This operation can be carried out under general or spinal anaesthesia. The latter is a regional anaesthetic anaesthetising the lower part of the body (as with an epidural). The anaesthetist will decide on the most suitable anaesthetic together with the patient.
Video of the operation
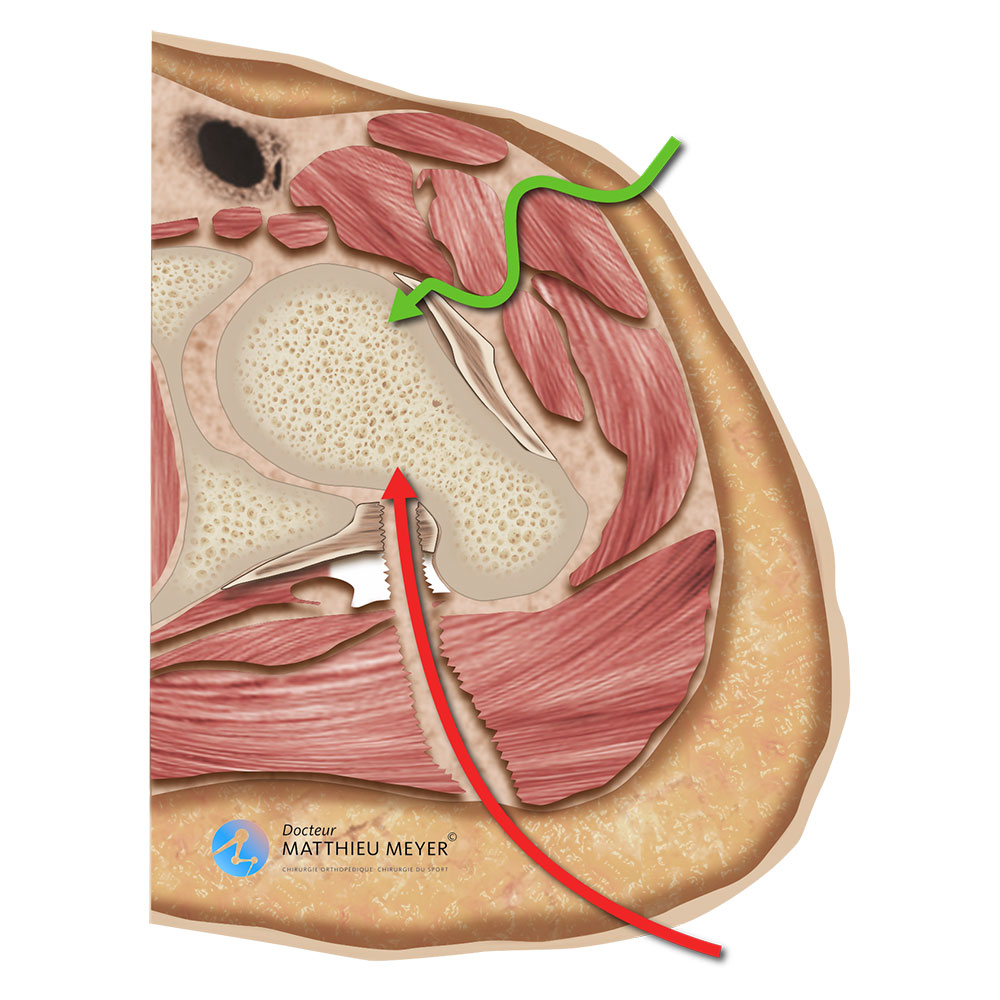
Hueter’s minimally invasive anterior approach
There are a variety of total hip replacement procedures. Hueter’s minimally invasive anterior approach has many advantages. Contrary to techniques currently used (Moore’s posterior approach, Harding’s anterior approach, transtrochanteric approach), this approach spares the surrounding anatomical structures, as the hip can be accessed without cutting any muscles, tendons, or bone.
Sparing the surrounding muscle is primordial as it ensures faster recovery and reduces the risk of dislocation of the implant. Moreover, this technique only requires a small incision that is often less than 8 centimetres long. The minimally invasive anterior approach can be used for the majority of patients for a primary total hip replacement. However, it is not always possible to treat extremely rare cases that may require a more extensive approach.
After the operation
Rehabilitation begins on the day of the operation or the following day with the help of physiotherapists. Except in specific cases, weight-bearing on the limb operated on is allowed from the outset. Crutches are used to start with but are gradually abandoned. Recovery is often faster with the minimally invasive anterior approach than with the other techniques and often provides greater stability when walking thanks to the preservation of the surrounding muscle.
The length of stay in hospital varies between 1 and 3 days; the operation is sometimes carried out as an outpatient procedure. When leaving the clinic, the patient can return home and rehabilitation will continue with a local physiotherapist with 2 to 3 sessions a week for about 1 month. If the patient’s home is too difficult to access or if the patient is old and has no help with daily activities (shopping, meals…) a stay of generally less than 3 weeks at a rehabilitation centre can be considered.
When the patient is discharged from the clinic, a consultation with follow-up x-rays of the implant is scheduled with the surgeon, generally 4 to 6 weeks after the operation, to ensure the patient has recovered good gait and hip mobility. A second check-up is generally recommended approximately 3 months after the operation. Check-up x-rays every few years are then recommended to ensure there is no abnormal wear of the implants or the surrounding bone.
Recovery after the operation
Recovery is often fast. Walking is resumed immediately but as a precaution, it is recommended to keep at least one stick for the first 2 weeks, longer if necessary.
Moderate inguinal pain is often felt during the first month then rapidly fades.
Driving can be resumed 2 to 4 weeks after the operation according to how the patient feels. Sports activities can be considered 2 to 3 months after the operation but preferably low-impact sports (cycling, swimming…).
Risks linked to the operation
Unfortunately, zero risk does not exist in surgery. Any operation has its risks and limitations, which you must accept or not undergo the operation. However, if an operation is proposed, the surgeon and the anaesthetist consider that the expected benefits far outweigh the risk incurred.
Some risks, such as microbial infections of the surgical site, are common to all types of surgery. Fortunately, this complication is rare but when it occurs requires the lavage of the prosthesis during another procedure and a course of antibiotics. More rarely, some infections may require the prosthesis to be replaced. Bruising can also appear around the surgical site. This is usually prevented or reduced with a suction drain inserted at the end of the operation and removed in the days following the operation. Exceptionally, a procedure may be required to reduce the pressure with severe bruising and a blood transfusion may sometimes be necessary in the case of severe bleeding.
Hip surgery also increases the risk of phlebitis, which can lead to a pulmonary embolism. To minimise this risk, blood thinners (in the form of daily injections or tablets) are prescribed for the entire month following the operation.
There are also risks specific to hip replacement surgery. Firstly, dislocation of the prosthesis is possible. Dislocation most often occurs in the first few weeks following the hip replacement when everything around it is not yet fully healed. When dislocated, a mild anaesthetic is necessary to put it back into place. It is also possible that the two legs are not the same length after the operation. This limb-length discrepancy is often well tolerated and goes unnoticed. However, if this is not the case and there is a limp, an insole may be prescribed.
Finally, rarer complications can also occur. A fracture of the femur can occur during the procedure, which generally delays the resumption of weight-bearing. Nerves can also be damaged accidentally during the operation with a risk of paralysis or loss of feeling in the limb operated on, which can be transitory or permanent.
If you have any concerns about the operation, do not hesitate to talk to your surgeon or the anaesthetist and they will answer any questions you may have.
A few questions about anterior approach hip replacements
What is the desired outcome of a total hip replacement?
A total hip replacement aims to restore satisfactory function of the hip joint. The aim is two-fold: eliminate the pain and restore joint mobility. Ultimately, most patients forget they have a hip prosthesis. However, this will vary according to the pathology that led to the hip replacement being carried out in the first place. In the case of some hip deformities, limping may persist due to an underlying muscular deficit.
My hip has been hurting for years. Do I need a hip replacement?
A hip replacement is a functional procedure and, therefore, elective. Only the patient can say whether the discomfort is considerable enough to justify an operation. However, if the wear is in the early stages, it is necessary to try medicinal treatments (analgesics, hyaluronic acid injections) to relieve the pain before considering surgery; this can often delay the hip replacement.
What is the lifespan of a hip prosthesis?
The lifespan of a primary hip prosthesis varies according to the type of prosthesis, the bearing surfaces, as well as how active the patient is (very active or sedentary). Nevertheless, it is reasonable to say that these days the lifespan of a hip replacement is approximately 20 years and probably longer with low-wear bearing surfaces such as ceramic with which the results are very promising.
Am I too young to undergo a total hip replacement?
The question behind this relates to the lifespan of the prosthesis, as revision hip surgery is more complicated and the functional result is unlikely to be as good as with the primary replacement. It is, therefore, preferable to perform hip replacements on patients who are never likely to have it changed, in other words, those over 65 years. Nevertheless, this is not set in stone. It is better to have a hip replacement at an age when you can enjoy it rather than delaying the procedure indefinitely and having to suffer with the pain and the frustration of restricted mobility. So, for subjects under 40 years with hip damage (aseptic osteonecrosis of the femoral head, for example), it is better to undergo a hip replacement to recover good quality of life rather than continue putting up with the pain for several years, especially as the bearing surfaces used in hip prostheses such as ceramic offer hope of longer lasting hip replacements.
What is the prosthesis made of?
Hip prostheses are made from inert biocompatible materials and so the risks of allergy or rejection are exceptional. The metal parts of the implants are alloys, more often than not cobalt-chromium or titanium. Cementless implants are generally coated in osteoconductive materials to facilitate growth of the bone in contact with the implant. The bearing surfaces of the prostheses, that is to say, the contact surfaces between the acetabulum and femur implants can be ceramic, metal, or polyethene (plastic). Low-wear bearing surfaces, especially ceramic (alumina), are currently used.
Are there any movements that should be avoided after a total hip replacement?
This is the great advantage of the minimally invasive anterior approach compared to other hip replacement techniques. With this technique, even if the risk of dislocation is not zero, it is much lower due to the preservation of the surrounding muscles and tendons. Furthermore, movements likely to result in the dislocation of the prosthesis are uncommon in daily life (extension and external rotation of the hip). Consequently, even if it is necessary to be careful during the first two months following the operation, this technique, contrary to the others, does not require you to sleep with a pillow between your legs and you are not prohibited from bending forward.
Do I need to make any changes at home after a total hip replacement?
No, it is not necessary. However, some accessories not considered essential can nevertheless make life more comfortable during the first few weeks after the operation, for example, a raised toilet seat.
Considering the advantages of the minimally invasive anterior approach, why isn’t it used more often by surgeons for hip replacements?
Although this technique is very old, the main reason why it is used so rarely is that until recently it was not very common and therefore taught little in university hospitals where surgeons train.
Where will the scar be?
With a minimally invasive anterior approach hip replacement, the scar is on the anterior surface of the joint, lengthwise or sometimes transversally within the groin crease (bikini scar), and is often less than 8 centimetres long. Its aesthetic appearance is often appreciated and can be improved with oil-rich creams to promote re-epidermisation and by protecting the scar from exposure to the sun in the two years following the operation.
Do I have to be totally unconscious during the operation?
No, this operation can be performed under regional anaesthetic if there are no contra-indications.
Is the operation painful?
Moderate pain will be experienced in the first few days after the operation that can be relieved with traditional analgesics and ice on the hip. However, the pain felt is very personal and therefore varies from one patient to another.
How long is the stay in hospital?
The length of stay generally varies between 1 and 3 days. In some circumstances, this operation can be carried out as outpatient procedure.
How long does it take to recover your independence?
Satisfactory independence is often recovered after 4 to 6 weeks.
How long after my operation can I travel again?
You have to wait between 2 and 3 months before taking a long journey in good conditions (carrying luggage, shuffling along during visits…).
When can I drive after the operation? Can I travel by car?
You will generally have to wait for 2 to 4 weeks after the operation before driving again. You can travel by car earlier but journeys are often uncomfortable due to the low sitting position and it is better to restrict the frequency and more particularly the duration.
How long will I be off work after the operation?
It depends on your profession and the level of physical activity required but generally varies between 1 and 3 months.
Can I do any sport after a hip replacement?
Yes, but it is better to opt for non-weight-bearing sports rather than high-impact sports. Cycling and swimming are therefore better but the experience of patients who did not stick to these recommendations has shown that sports that put more strain on the prosthesis such as skiing are possible. Sport is generally not resumed before the 3rd month after the operation.
What are the risks linked to a total hip replacement?
Unfortunately, zero risk does not exist in surgery. Any operation has its risks and limitations, which you must accept or not undergo the operation. However, if an operation is proposed, the surgeon and the anaesthetist consider that the expected benefits far outweigh the risk incurred.
Some risks, such as microbial infections of the surgical site, are common to all types of surgery. Fortunately, this complication is rare but when it occurs requires the lavage of the prosthesis during another procedure and a course of antibiotics. More rarely, some infections can require the prosthesis to be replaced. Bruising can also appear around the surgical site. This is usually prevented or reduced with a suction drain inserted at the end of the operation and removed in the days following the operation. Exceptionally, a procedure may be required to reduce the pressure with severe bruising and a blood transfusion may sometimes be necessary in the case of severe bleeding.
Hip surgery also increases the risk of phlebitis, which can lead to a pulmonary embolism. To minimise this risk, blood thinners (in the form of daily injections or tablets) are prescribed for the entire month following the operation.
There are also risks specific to hip replacement surgery. Firstly, dislocation of the prosthesis is possible. Dislocation most often occurs in the first weeks following the hip replacement when everything around it is not yet fully healed. When dislocated, a mild anaesthetic is necessary to put it back into place. It is also possible that the two legs are not the same length after the operation. This limb-length discrepancy is often well tolerated and goes unnoticed. If this is not the case and there is a limp, an insole may be prescribed.
Finally, rarer complications can also occur. A fracture of the femur can occur during the procedure, which generally delays the resumption of weight-bearing. Nerves can also be damaged accidentally during the operation with a risk of paralysis or loss of feeling in the limb operated on, which can be transitory or permanent.
If you have any concerns about the operation, do not hesitate to talk to your surgeon or the anaesthetist and they will answer any questions you may have.
In summary...
when is surgery necessary?
When the pain is too much and medication no longer provides enough relief
aim of the operation
Disappearance of the pain / Recovery of hip mobility and walking
which anaesthesia?
General or regional determined during the pre-operative anaesthesia consultation
Duration of hospitalisation
Between 1 and 3 days, operation sometimes performed in an outpatient setting
resumption of weight-bearing
From the day of the operation or the following day, using crutches to start with
after the operation
Return home in most cases, discharge to a reahabilitation centre for extremely isolated patients or home difficult to access
duration of rehabilitation
Generally, 1 month
Duration of medical leave
1 to 3 months
resumption of car driving
2 to 4 weeks after the operation
Resumption of sport
3 months after the operation preferably non-weight-bearing sports
Make an appointment
please do not hesitate to contact us or make an appointment online via DoctoLib