In Summary...
Who requires surgery?
Recent PCL lesions if combined with peripheral ligaments. Old lesions if knee unstable or bothersome patellar pain
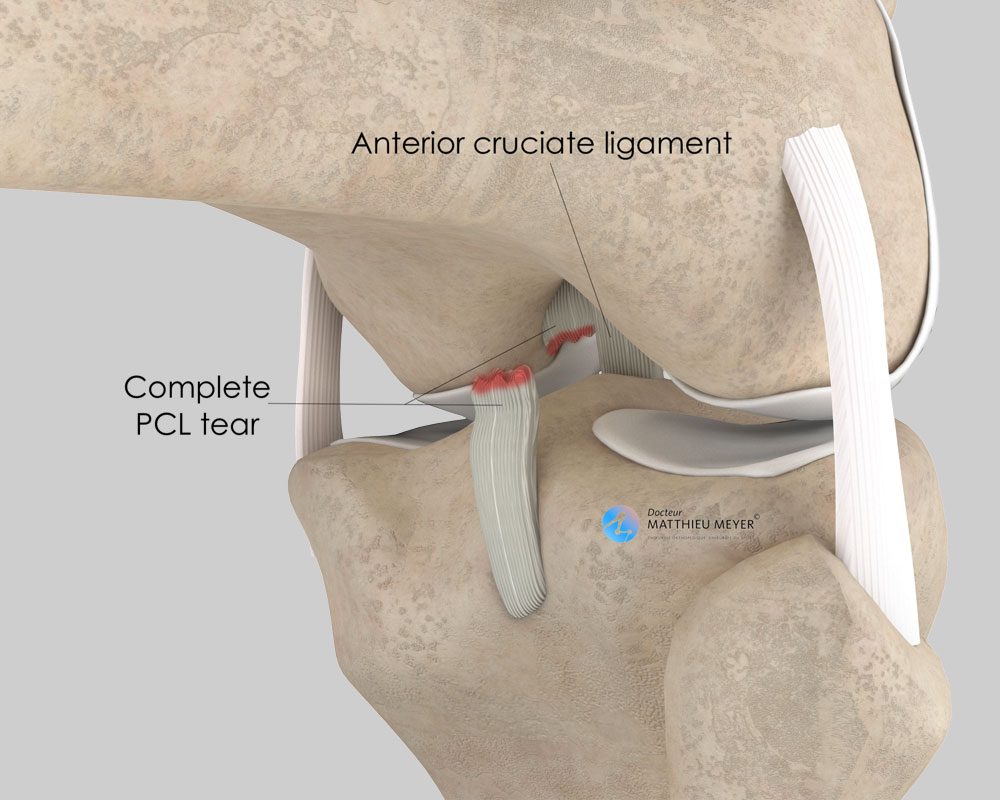
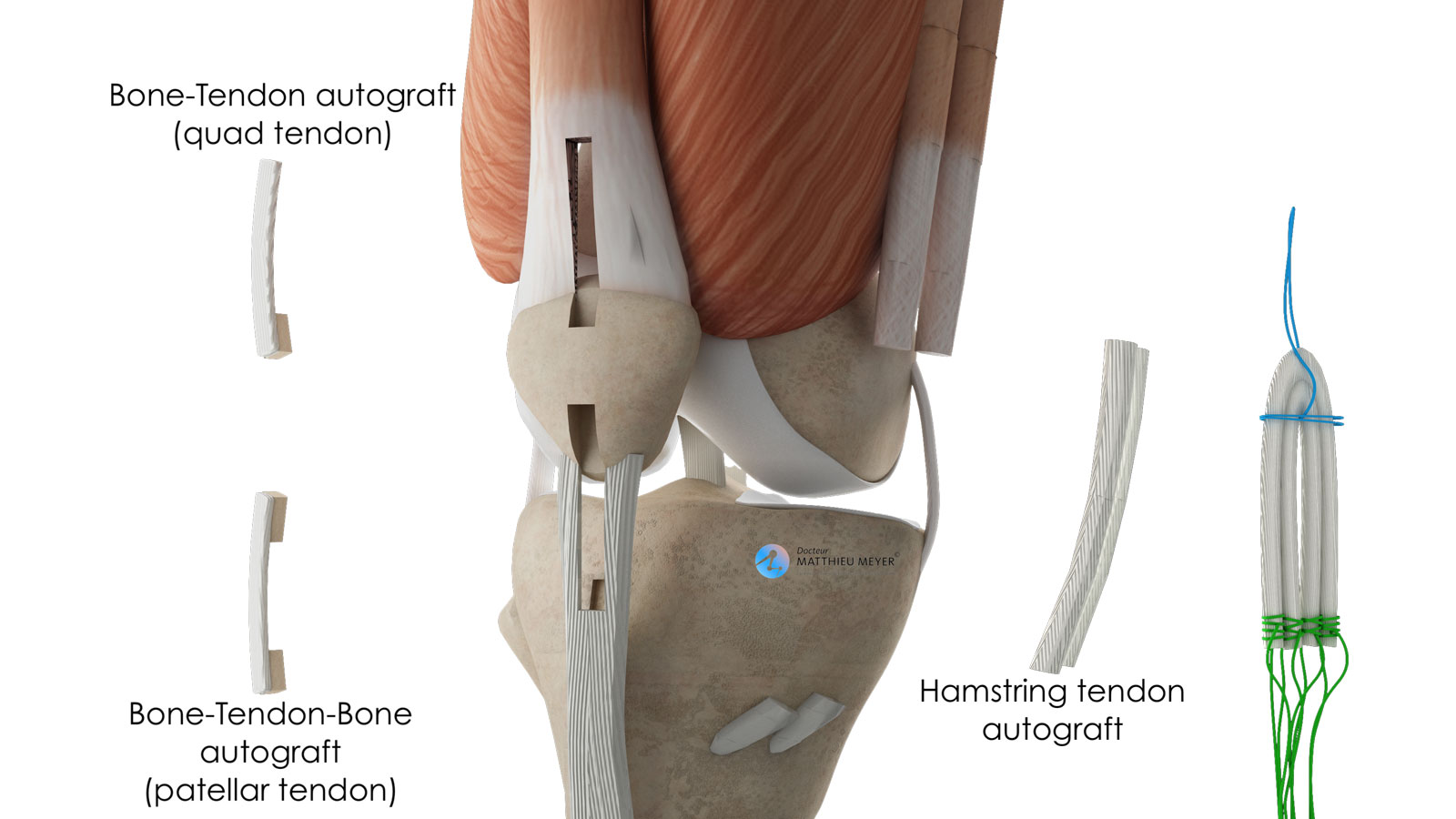
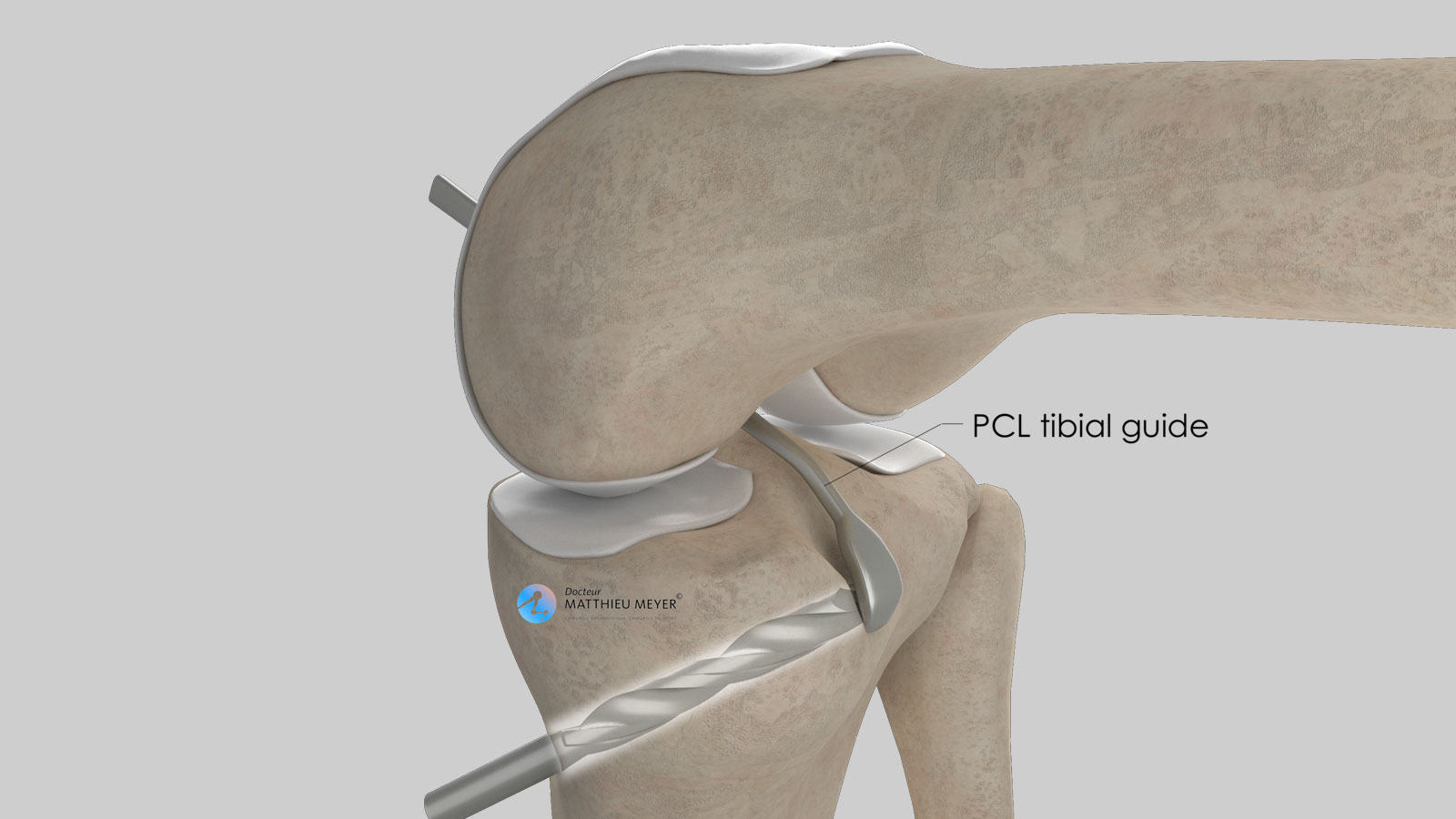
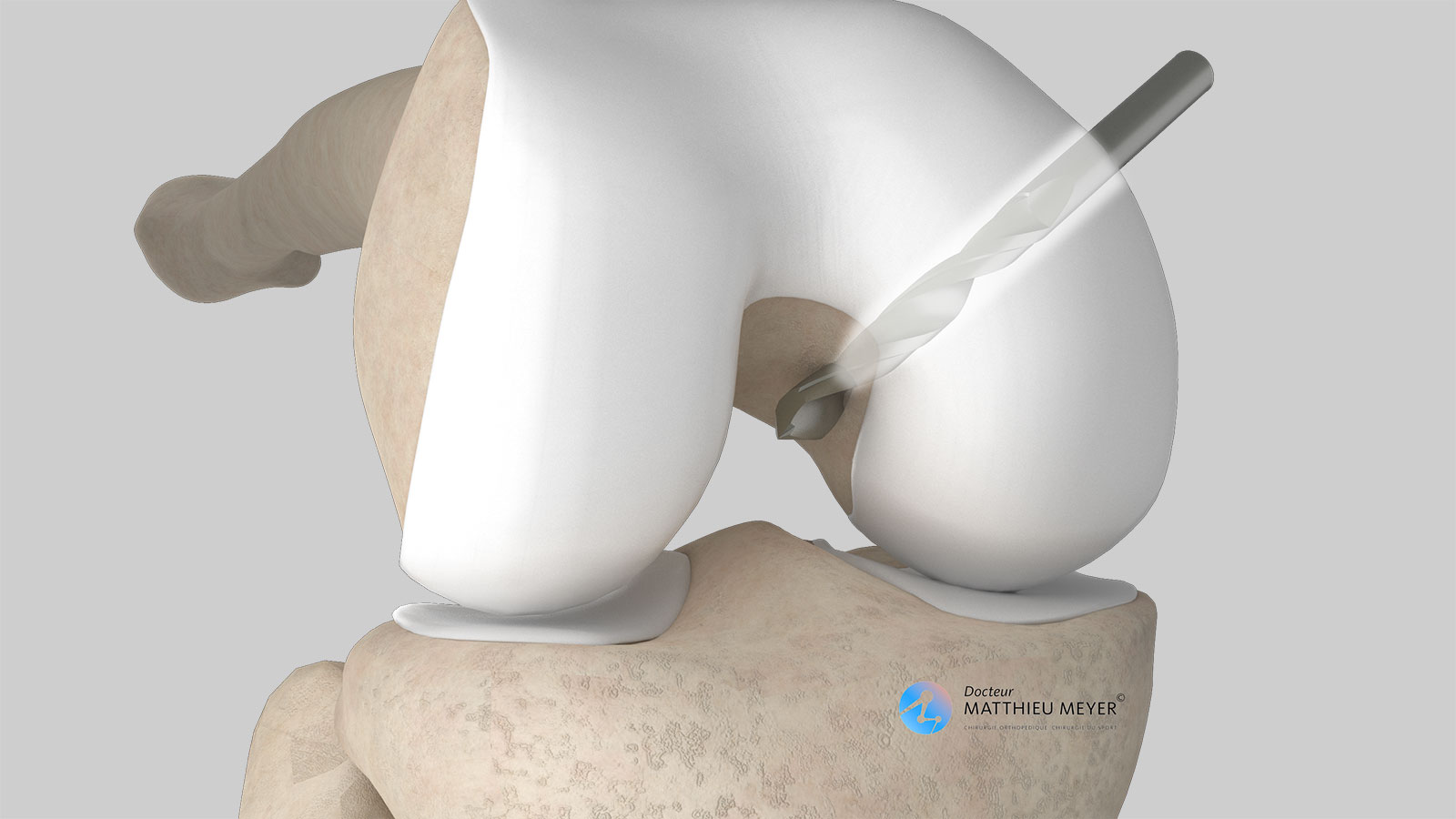
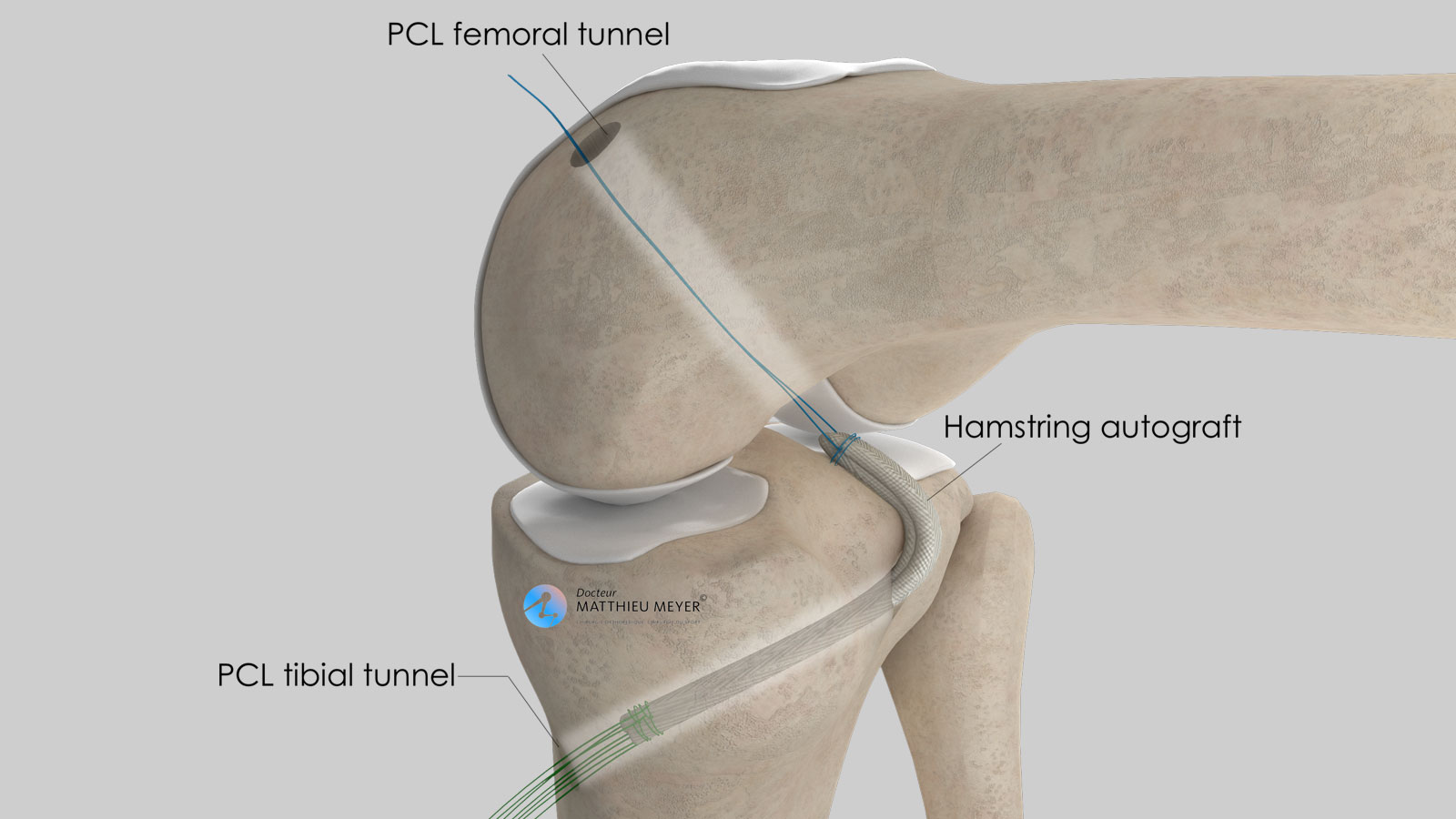
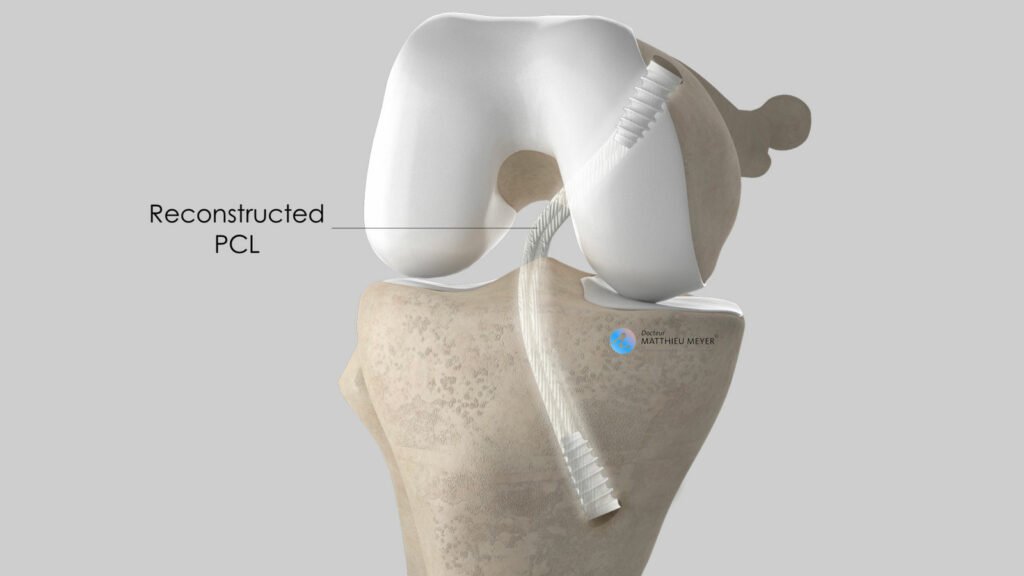
Surgical technique
Arthroscopy for PCL
Which anaesthesia?
General or regional according to the patient’s history and wishes (determined with the anaesthetist)
Duration of hospitalisation
Outpatient surgery or 1 to 2 nights at the clinic (longer in the case of damage to several ligaments)
Resumption of weight-bearing
Immediate alleviated with crutches for 3 weeks
Duration of medical leave
1 to 3 months depending on the profession
Resumption of car driving
6 weeks after the operation
Resumption of riding a motorbike
4 months after the operation
Resumption of sport
Progressive from the 3rd month after the operation and from the 9th month for pivoting sports