Total Shoulder Replacement
Home » Operations » Shoulder Surgery » Painful Shoulder » Total Shoulder Replacement
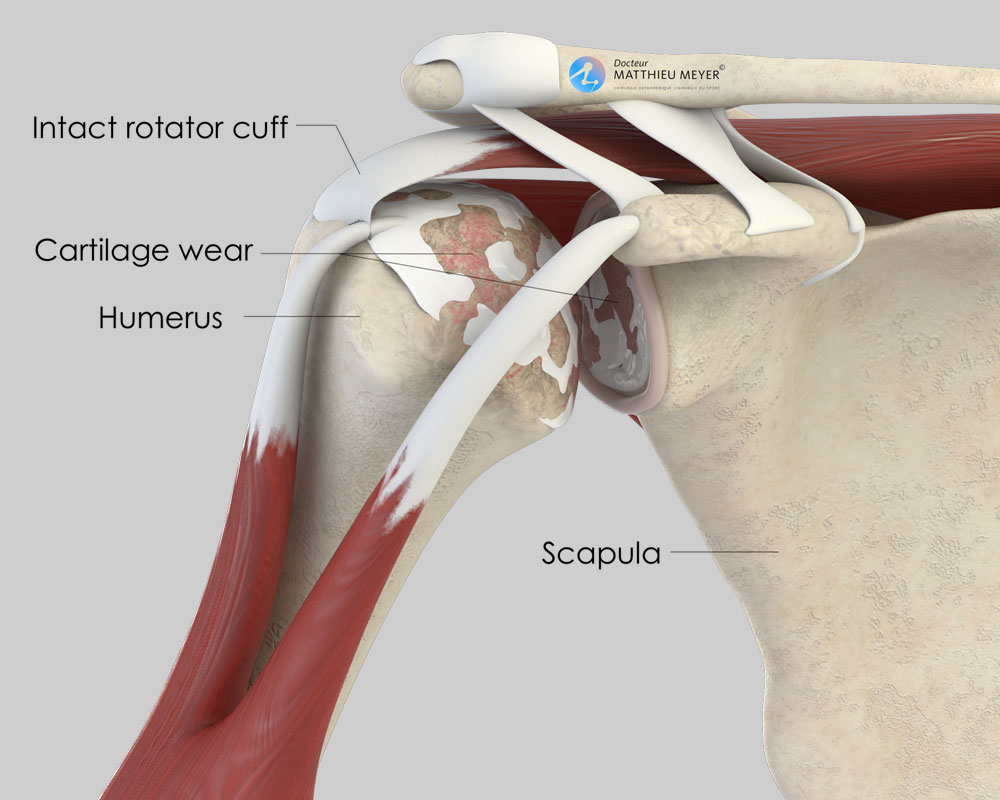
A shoulder replacement aims to replace the glenohumeral joint located between the scapula (shoulder blade) and the humerus (arm bone).
Normal shoulder function
To move, the glenohumeral joint needs the muscles and tendons intact.
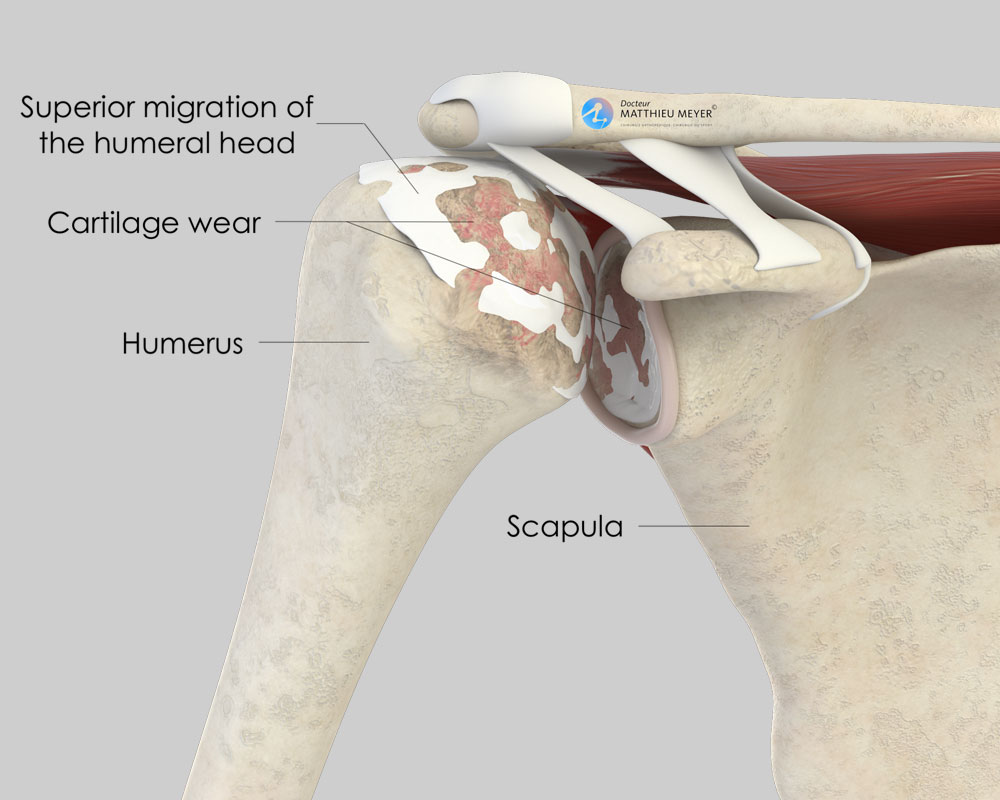
The main muscles are the deltoid and rotator cuff muscles. The deltoid enables anterior, posterior, and lateral elevation, and generally remains intact with ageing. The rotator cuff muscles enable lateral elevation and rotation of the arm. With ageing, they can tear totally or partially.
The cartilage is an extremely slippery substance with no nerve endings that allows the joint to move freely and painlessly. For different reasons (osteoarthritis, rheumatism, osteonecrosis of the head of the humerus…) this cartilage can wear exposing the underlying bone, which is rough and innervated, and the joint gradually becomes stiff and painful.
Indications for a shoulder replacement
A shoulder replacement may be necessary for the following 3 indications:
- Joint cartilage damage (osteoarthritis, osteonecrosis of the humeral head, rheumatism, sequelae of fractures or an infection)
- Fractures of the humeral head with a high risk of bone necrosis
- Paralytic shoulder as a result of unrepairable rotator cuff tendon tears
The different types of shoulder replacement
There are different types of shoulder replacement:
- A partial shoulder replacement involves replacing only the damaged humeral head (osteonecrosis or fracture of the humeral head) and the glenoid fossa of the shoulder blade is left intact
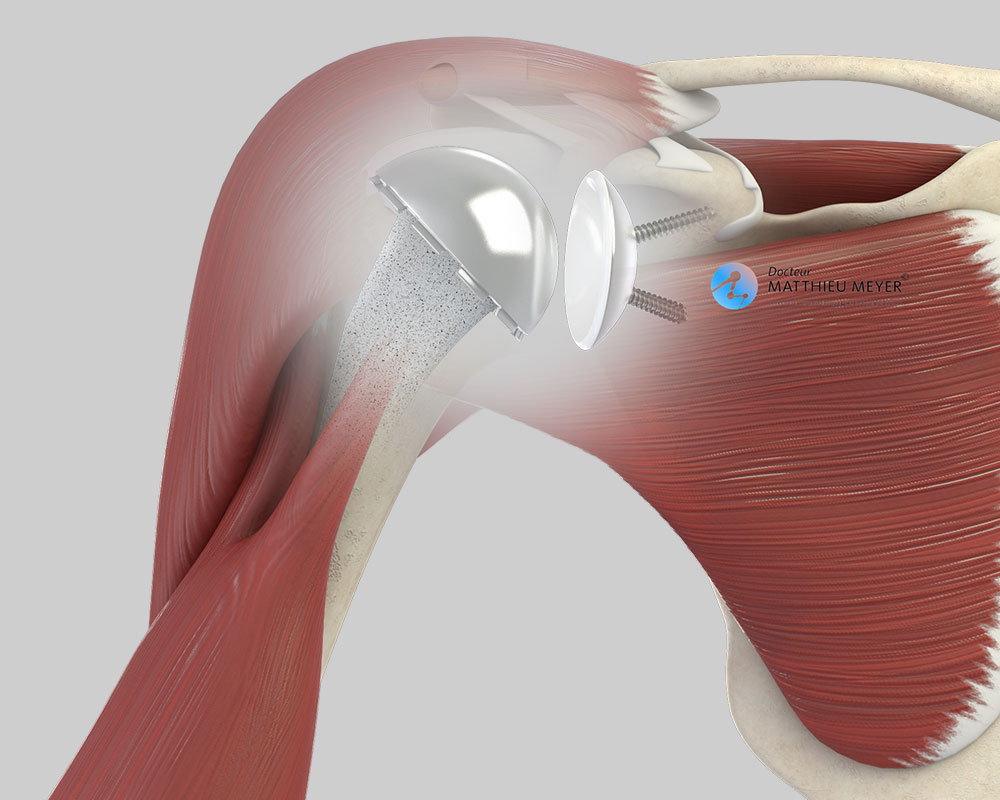
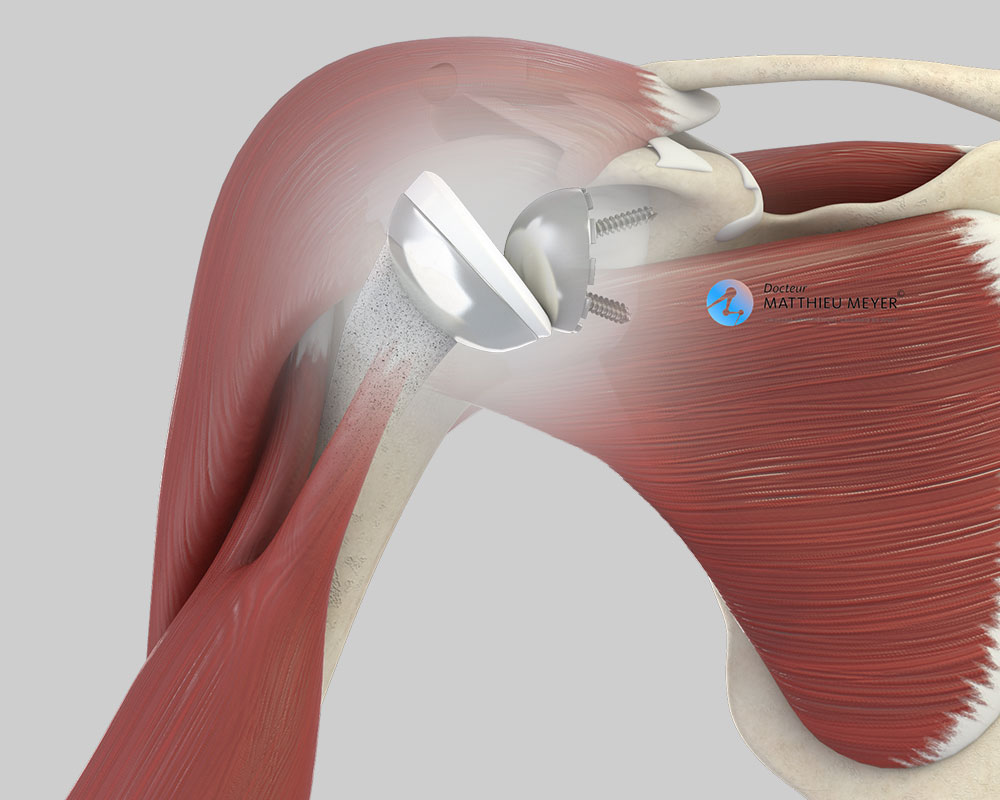
- A total shoulder replacement involves replacing both the cartilage on the shoulder blade and the humeral head. There are two types of total shoulder replacement:
- Standard shoulder replacement, which is indicated when the shoulder muscles are intact. This type of total replacement provides the best results in terms of range of motion and durability.
- Reverse shoulder replacement, which is indicated when the shoulder muscles are damaged. This is a palliative solution for which the results are not as good as a standard total shoulder replacement in terms of range of motion and durability and can only be performed when the shoulder muscles are damaged.
To move, the prosthesis requires muscles. When all the shoulder muscles are intact, a standard replacement is carried out with an anatomical prosthesis corresponding to the natural shape of the shoulder.
However, when the rotator cuff is damaged, the outcome of this type of replacement is poor. In this case, a reverse replacement is preferred of which the position helps the remaining muscles work more effectively thus enabling recovery of greater shoulder range of motion.
A reverse replacement can also be proposed when the cartilage is not damaged but the shoulder can no longer move due to a rotator cuff tear, as in this case the replacement will help the deltoid muscle and enable recovery of a little shoulder mobility.
The operation
A shoulder replacement requires an operation and the type of prosthesis best suited to the patient is chosen during pre-surgical consultations. Before the operation, a pre-anaesthesia consultation and a preoperative assessment are conducted to check the patient is physically apt to undergo the operation and minimise the risk of postoperative complications, especially infections. This assessment generally includes a blood test, a cardiovascular check-up, as well as a dental check-up and a urine test to ensure there are no infections and thus avoid any microbial contamination of the prosthesis.
The operation generally lasts between 1 and 2 hours plus the time required for the anaesthetic and positioning the patient on the operating table. This operation is carried out under general anaesthesia. The anaesthetist can also anaesthetise the upper limb from the shoulder to the hand with a regional anaesthetic. This additional anaesthetic, known as an interscalene nerve block, lasts longer than a general anaesthetic and helps prevent immediate postoperative pain.
The prosthesis is fitted through an incision about 10 centimetres long on the anterior side of the shoulder above the armpit.
Rehabilitation begins the day after the operation with the help of physiotherapists. Some movements are allowed from the outset, others later. A shoulder brace is often required for 6 weeks after the procedure to allow the shoulder tendons to heal. However, this brace can be removed during the day but proscribed movements specified by the surgeon must be avoided.
The stay in hospital is often between 2 and 4 days. The patient can return home when discharged. The rehabilitation sessions will be carried out with a local physiotherapist or at a rehabilitation centre as an outpatient.
When the patient is discharged from the clinic, a consultation with follow-up x-rays of the implant is scheduled with the surgeon 4 to 6 weeks after the operation to check the shoulder has recovered well. Other consultations will then be scheduled of which the number and frequency will depend on how rapidly the patient recovers. X-rays to monitor the replacement are recommended, generally every 2 years, to check there is no abnormal wear of the implants or the surrounding bone.
A few questions about shoulder replacements
What is the desired outcome of a shoulder replacement?
A shoulder replacement aims to restore painless shoulder function and mobility. However, it is not possible to recover a “normal” shoulder. A shoulder replacement is less mobile than a natural shoulder, especially reverse replacements for which rotational movements are very restricted and can hinder bottom hygiene.
I have had shoulder osteoarthritis for several years. Do I need a shoulder replacement?
A shoulder replacement is a functional procedure and therefore not compulsory. Only the patient can say if the discomfort is considerable enough to justify an operation. However, before considering surgery, it is necessary to try relieving the pain with medicinal treatments (analgesics, hyaluronic acid injections), which can often delay a shoulder replacement.
What is the lifespan of a shoulder replacement?
87% of standard shoulder replacements are still in place after 15 years.
Concerning reverse shoulder replacements, for which there is less long-term data, the 10-year survival rate is 95%.
What is the prosthesis made of?
Shoulder implants are made from inert biocompatible materials and so the risks of allergy or rejection are exceptional. The metal parts of the implants are alloys, more often than not cobalt-chromium or titanium. Cementless implants are generally coated in osteoconductive materials to facilitate the growth of the bone in contact with the implant.
When can I drive after the operation?
You will generally have to wait for 6 to 8 weeks after the operation before driving again.
How long will I be off work after the operation?
It depends on your profession and the level of physical activity required but generally varies between 2 and 6 months. For some manual or physical work, a change in profession must be considered.
Can I do any sport with a shoulder replacement?
Yes, sport can be resumed with a shoulder replacement. However, it should be limited and not before the 6th month after the operation. Throwing and contact sports must be avoided as they can result in the premature wear of the implant. Sports with a high risk of falling must also be avoided to prevent any risk of fracturing the bone surrounding the prosthesis.
What are the risks linked to a total shoulder replacement?
Unfortunately, zero risk does not exist in surgery. Any operation has its risks and limitations, which you must accept or not undergo the operation. However, if an operation is proposed, the surgeon and the anaesthetist consider that the expected benefits far outweigh the risk incurred.
Some risks, such as microbial infections of the surgical site, are common to all types of surgery. This complication is fortunately rare but when it occurs requires another operation and a course of antibiotics. Some infections may require the implants to be replaced. Bruising can also appear around the surgical site. This is usually prevented or reduced with a suction drain inserted at the end of the operation and removed in the days following the procedure. However, in the case of severe bleeding during or following the operation, another operation to stop the haemorrhage or a blood transfusion may be required.
There are also risks specific to shoulder replacement surgery. Firstly, dislocation of the prosthesis is possible. Dislocation most often occurs in the first few weeks following the shoulder replacement when everything around it has not yet fully healed. When dislocated, a mild anaesthetic is necessary to put it back into place.
Finally, rarer complications can also occur. A fracture of the humerus can occur during the procedure. Nerves can also be accidentally damaged during the operation with a risk of paralysis or loss of feeling in the limb operated on, which can be transitory or permanent.
If you have any concerns about the operation, do not hesitate to talk to your surgeon or the anaesthetist and they will answer any questions you may have.
In summary...
When is surgery necessary?
When the pain is too intense and medication no longer provides enough relief
Aim of the operation
Eliminate the pain / Recover shoulder mobility
Which anaesthesia?
General with an interscalene nerve block for postoperative pain management
Duration of hospitalisation
Between 2 and 4 days
After the operation
Return home
Duration of rehabilitation
Between 3 and 6 months
Duration of medical leave
Between 2 and 6 months according to the patient’s profession
Resumption of car driving
2 months after the operation
Resumption of sport
6 months after the operation
(no throwing or contact sports)
Make an appointment
please do not hesitate to contact us or make an appointment online via DoctoLib