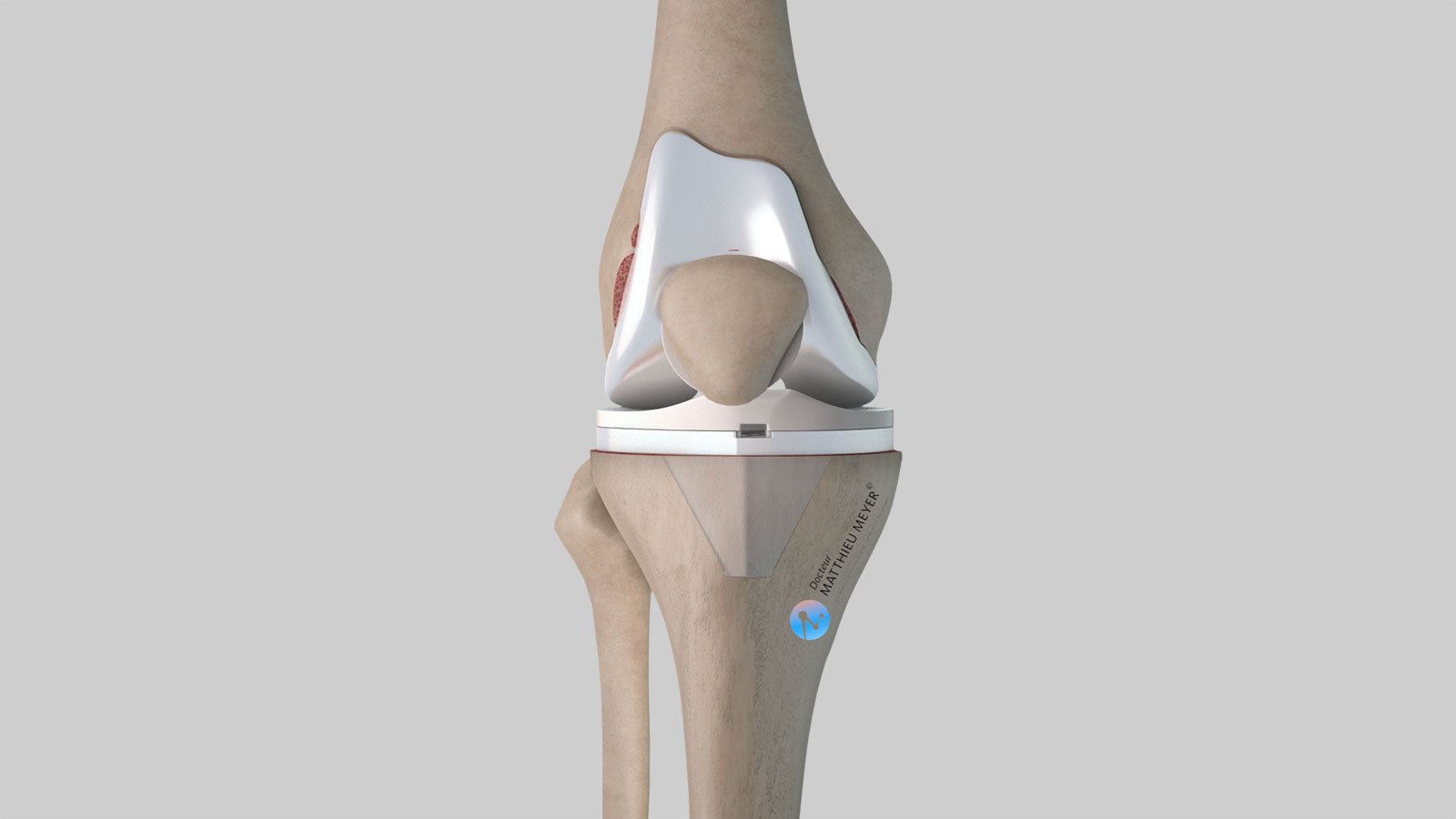
What is the desired outcome of a total knee replacement?
A total knee replacement aims to restore satisfactory function of the knee joint. The aim is two-fold: eliminate the pain and restore joint mobility. A total knee replacement helps recover satisfactory, painless walking. However, the range of motion of an artificial knee is lower than a normal knee and is often between 110° and 130°, which enables normal walking even on stairs. Additionally, it is often uncomfortable to kneel on a hard floor with a knee replacement, which can hinder some activities.
Can we forget that we have a knee prosthesis?
Contrary to a hip replacement, it is rare that patients totally forget they have a knee replacement. Indeed, even if the knee is painless, odd feelings are often experienced especially when the weather changes but no specific treatment is required.
A TKR or a PKR?
You do not have to choose as these two types of replacement have clearly different indications (limited cartilage wear for a PKR and diffuse wear for a TKR) and some contra-indications (obesity, ligament problems or extension deficit of articular origin for PKR). The surgeon will decide on the most suitable prosthesis for the patient.
Can the deterioration of knee osteoarthritis be slowed to delay the need for a total knee replacement?
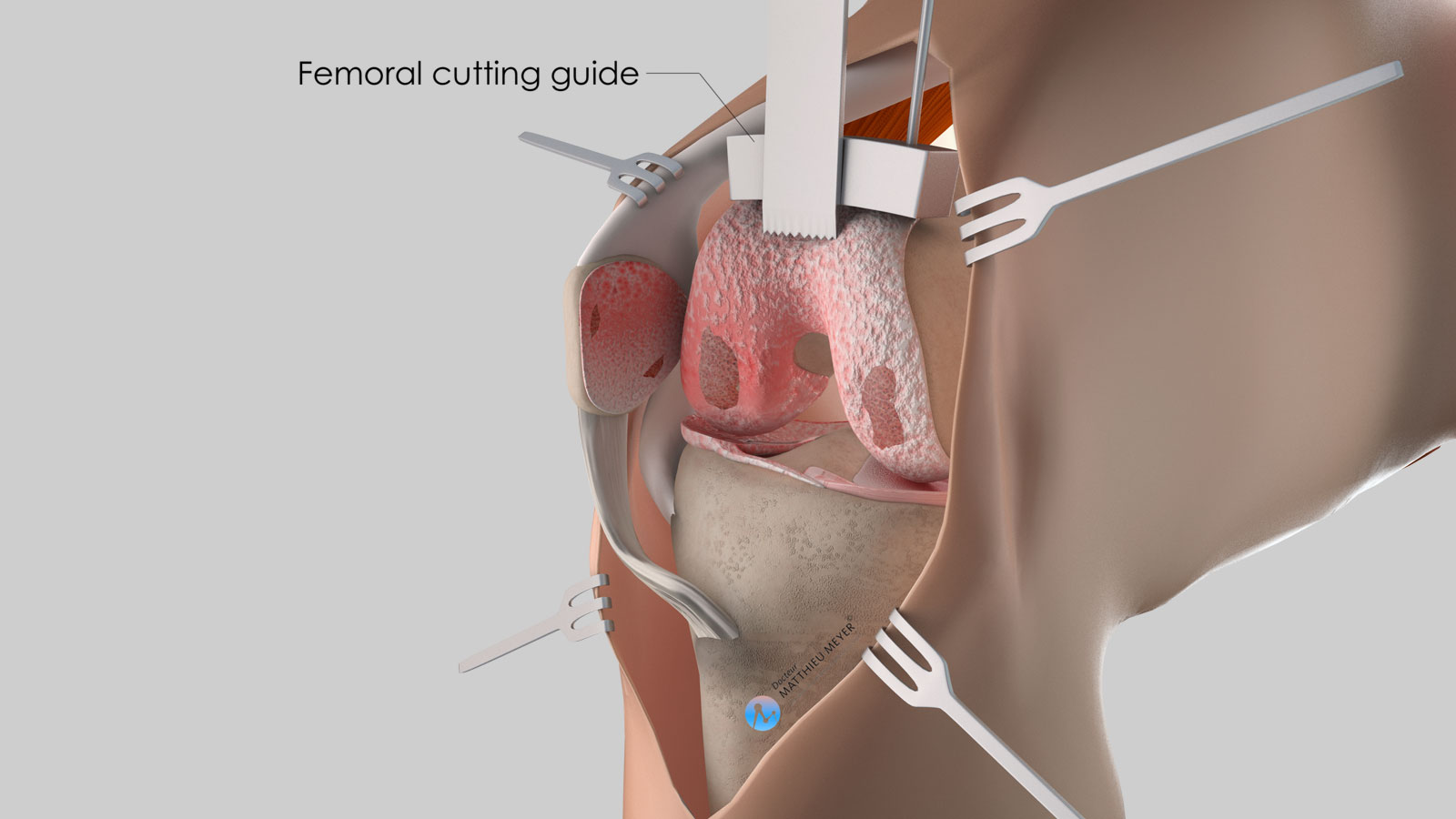
In some cases, conservative surgery (with no implant), of which the aim is to modify the mechanical load on the knee, can slow the progression of moderate, localised knee cartilage wear. The knee axis is modified slightly by realigning the proximal end of the tibia (high tibial osteotomy) or the distal end of the femur (distal femoral osteotomy). This transfers the load from the worn femorotibial compartment to the healthy femorotibial compartment. This type of operation does not heal the worn cartilage but slows the wear and thus delays the need for a knee replacement.
My knee has been hurting for years. Do I need a knee replacement?
A knee replacement is a functional procedure and therefore not compulsory. Only the patient can say if the discomfort is considerable enough to justify an operation. However, before considering surgery, it is necessary to try relieving the pain with medicinal treatments (analgesics, hyaluronic acid injections). In young patients, conservative surgery is sometimes possible to delay a knee replacement.
What is the lifespan of a knee replacement?
The lifespan of a primary knee replacement varies according to the type of implant, the bearing surfaces of the prosthetic joint, but also how active the patient is (very dynamic or sedentary). However, today it is reasonable to say that the lifespan of a knee replacement is approximately 20 to 25 years, sometimes longer, sometimes shorter.
Am I too young to have a total knee replacement?
Behind this question lies the issue of the lifespan of the implant and the potential need for a revision knee replacement as it is more complicated and the functional result is not likely to be as good as the primary replacement. It is, therefore, preferable to carry out knee replacements on patients who are never likely to have it changed, in other words, those over 65 years. Nevertheless, this is not set in stone. It is better to have a knee replacement at an age when you can enjoy it rather than delaying the procedure indefinitely and having to suffer the pain and the frustration of restricted mobility. So, for subjects under 50 with knee damage (sequelae of trauma, for example), it is better to undergo a knee replacement to recover satisfactory function rather than continuing to suffer from the pain for several years and finally undergoing a knee replacement a few years later.
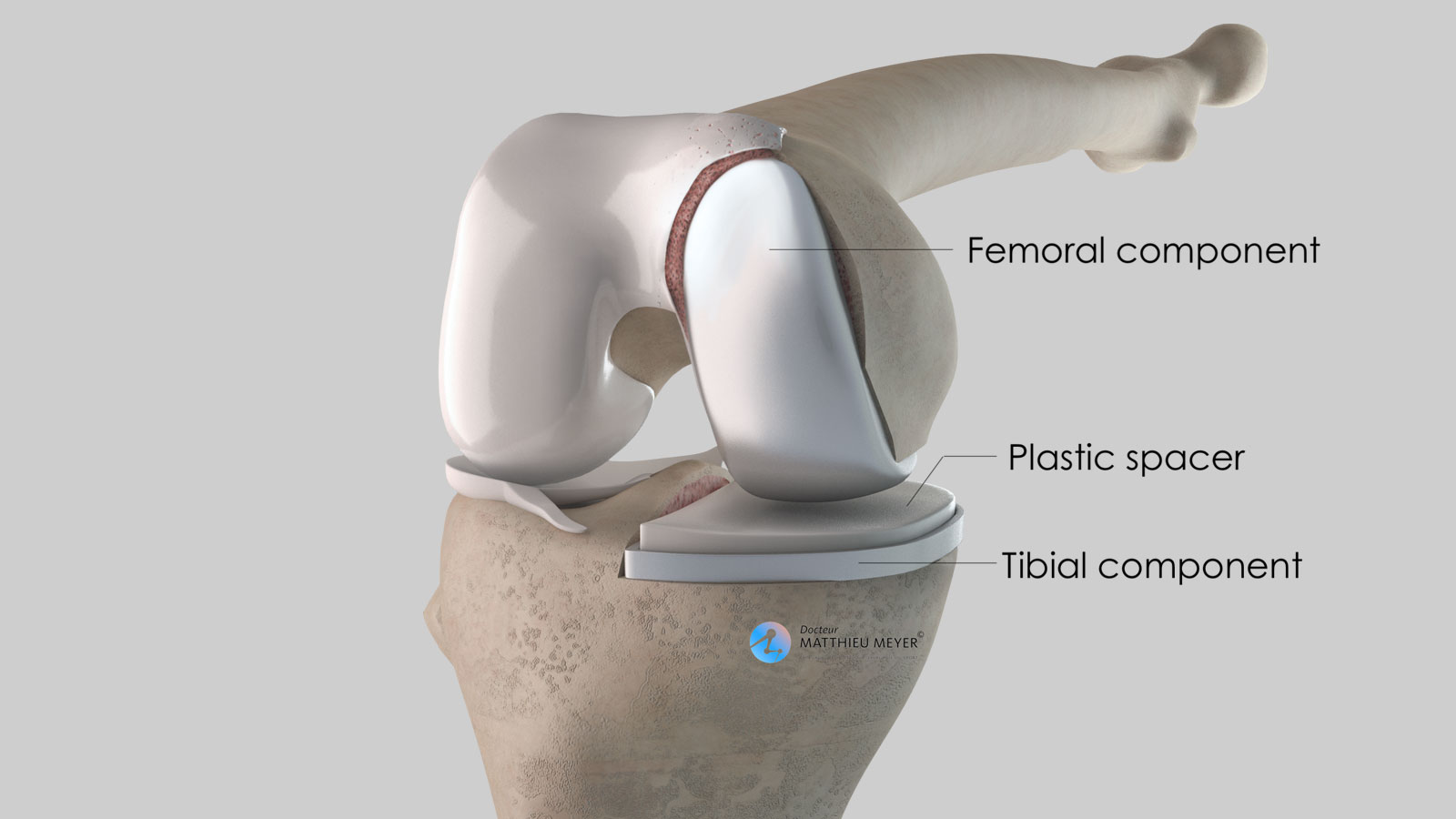
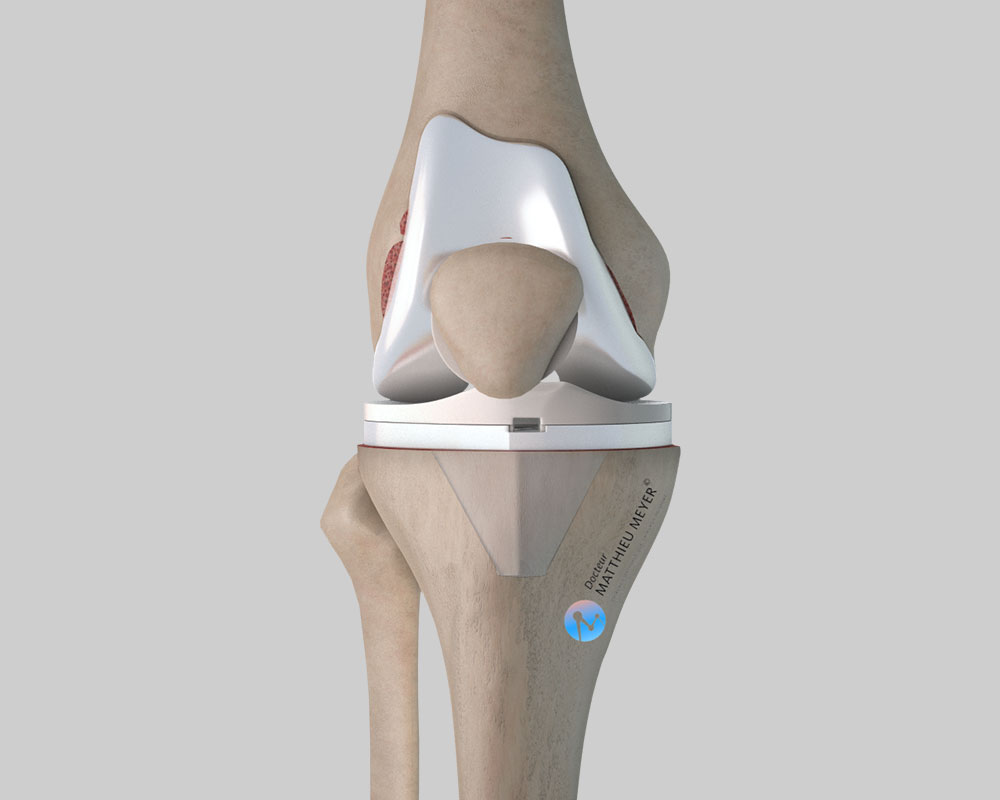
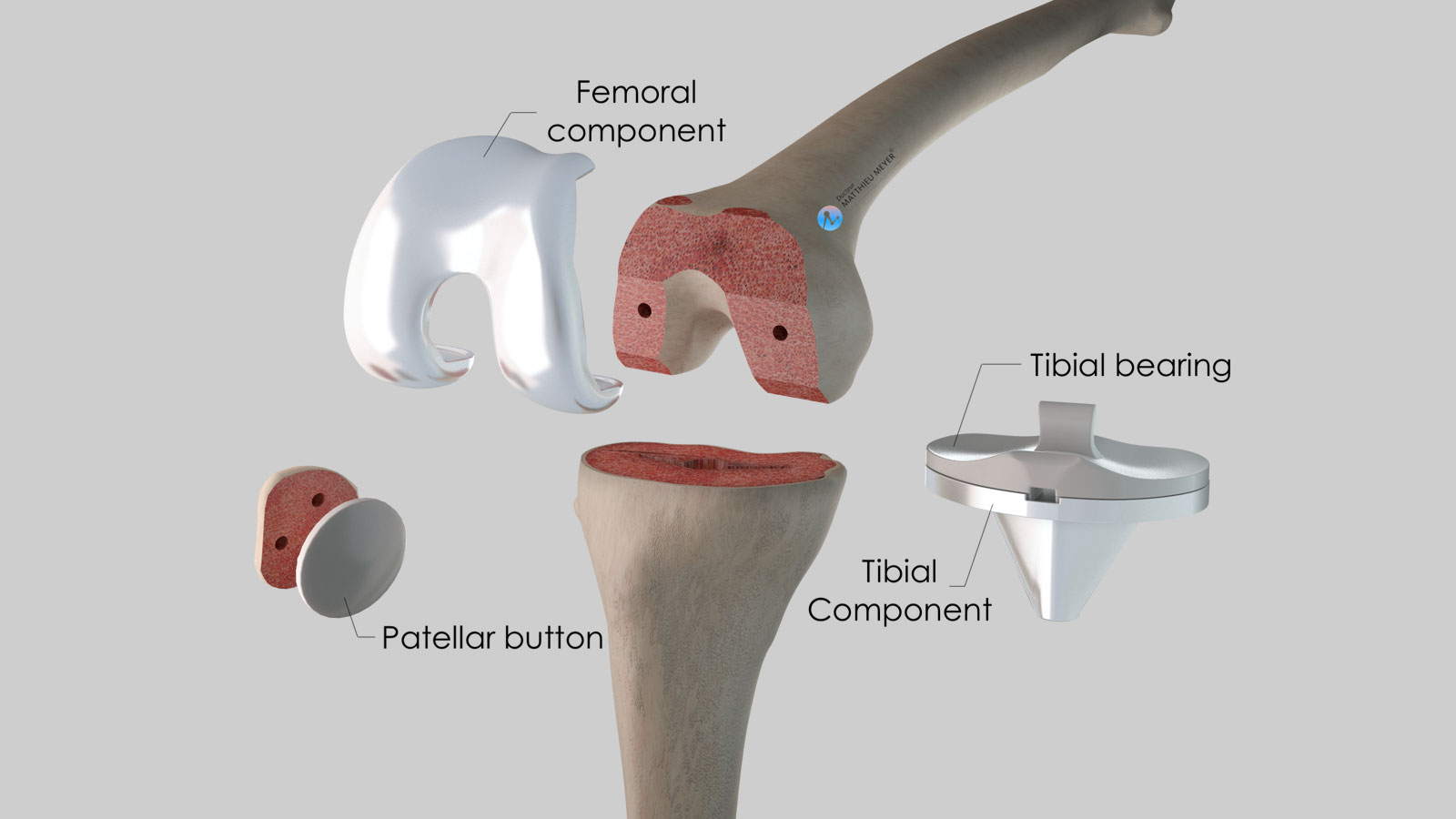
What is the implant made of?
Knee implants are made from inert biocompatible materials, so the risk of an allergy or rejection is exceptional. The metal parts of the implants are alloys, more often than not cobalt-chromium or titanium. Cementless implants are generally coated in osteoconductive materials to facilitate growth of the bone in contact with the implant. The bearing surfaces of the implants, that is the contact surfaces between the implants, are generally metal on polyethene (plastic).
Do I need to make any changes at home after a total knee replacement?
No, it is not necessary. However, ground-floor accommodation would be more comfortable in the first weeks after the operation.
Where will the scar be?
The scar is on the anterior surface of the knee and is generally between 10 and 15 cm.
Can I put weight on the knee straight after the operation?
Yes, weight-bearing on the limb operated on is resumed straight away.
How long does it take to recover your independence?
Satisfactory independence is often recovered after 4 to 6 weeks.
How long after my operation can I travel again?
You have to wait approximately 3 months before taking a long journey in good conditions (carrying luggage, shuffling during visits…)
When can I drive after the operation? Can I travel by car?
You will generally have to wait 4 to 6 weeks after the operation before driving again. When driving again, you must be able to do an emergency stop. You can travel as a passenger earlier but journeys are often uncomfortable due to the low sitting position and it is better to restrict the frequency and more particularly the duration.
How long will I be off work after the operation?
It depends on your profession and the level of physical activity required but generally varies between 2 and 3 months.
Can I do any sport with a knee implant?
Yes, but it is better to opt for non-weight-bearing sports rather than high-impact sports. Cycling and swimming are therefore better and running should be avoided. To be on the safe side, sport is generally not resumed before the 3rd month after the operation.
What are the risks linked to a total knee replacement?
Unfortunately, zero risk does not exist in surgery. Any operation has its risks and limitations, which you must accept or not undergo the operation. However, if an operation is proposed, the surgeon and the anaesthetist consider that the expected benefits far outweigh the risk incurred.
Some risks, such as microbial infections of the surgical site, are common to all types of surgery. Fortunately, this complication is rare but when it occurs requires another operation and a course of antibiotics. Some infections may require the implants to be replaced. Bruising can also appear around the surgical site. This is usually prevented or reduced with a suction drain inserted at the end of the operation and removed in the days following the operation. However, in the case of severe bleeding during or following the operation, another operation to stop the haemorrhage or a blood transfusion may be required.
Knee surgery also increases the risk of phlebitis, which can lead to a pulmonary embolism. To minimise this risk, blood thinners (in the form of daily injections or tablets) are prescribed for the entire month following the operation.
In rare cases, the knee remains stiff, hot, and painful for several months after the operation. This complication, known as algodystrophy or Chronic Regional Pain Syndrome (CRPS), is unpredictable and sometimes takes a long time to heal.
Finally, rarer complications can also occur. Blood vessels (arteries, veins) can be accidentally damaged and will require vascular surgery (bypass). Nerves can also be damaged accidentally during the operation with a risk of paralysis or loss of feeling in the limb operated on, which can be transitory or permanent.
If you have any concerns about the operation, do not hesitate to talk to your surgeon or the anaesthetist and they will answer any questions you may have.