Acromioclavicular Dislocation
Home » Operations » Shoulder Surgery » Traumatic Shoulder Injuries » Acromioclavicular Dislocation
Understanding acromioclavicular dislocation
The shoulder comprises the clavicle and the scapula, which connect the arm to the rib cage.
The clavicle is not very mobile as the medial end is solidly attached to the sternum by strong ligaments. This is known as the sternoclavicular joint.
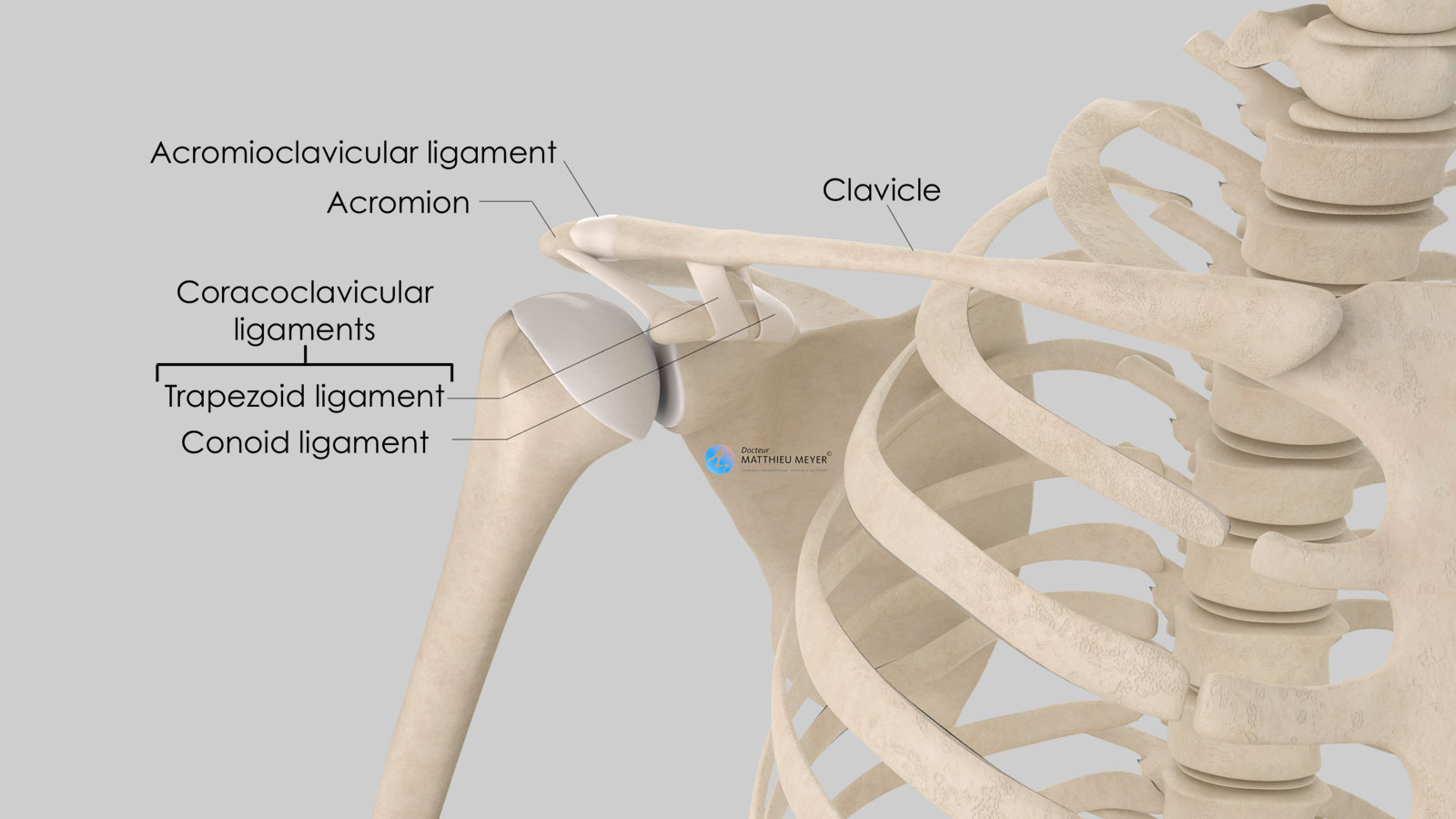
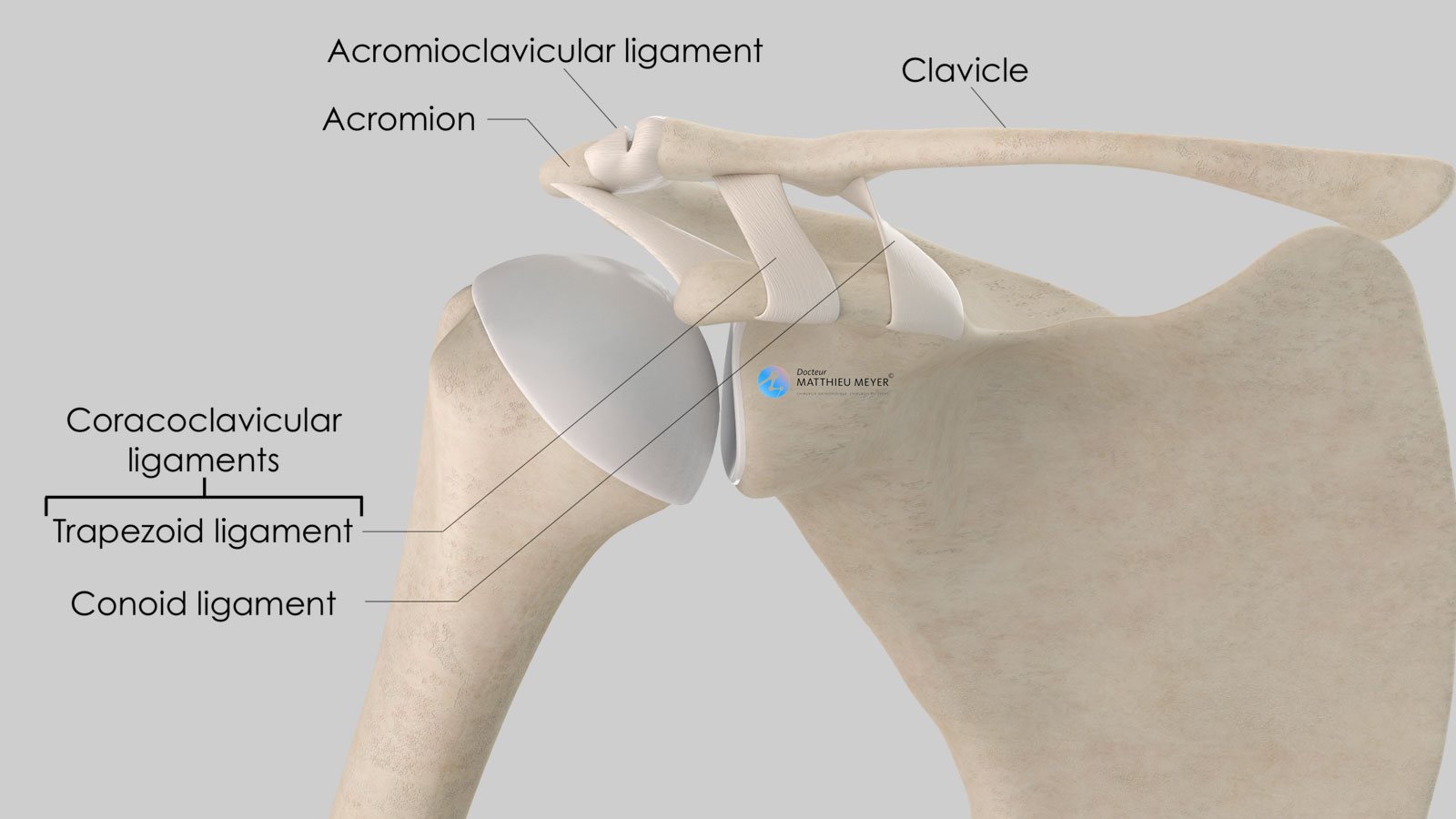
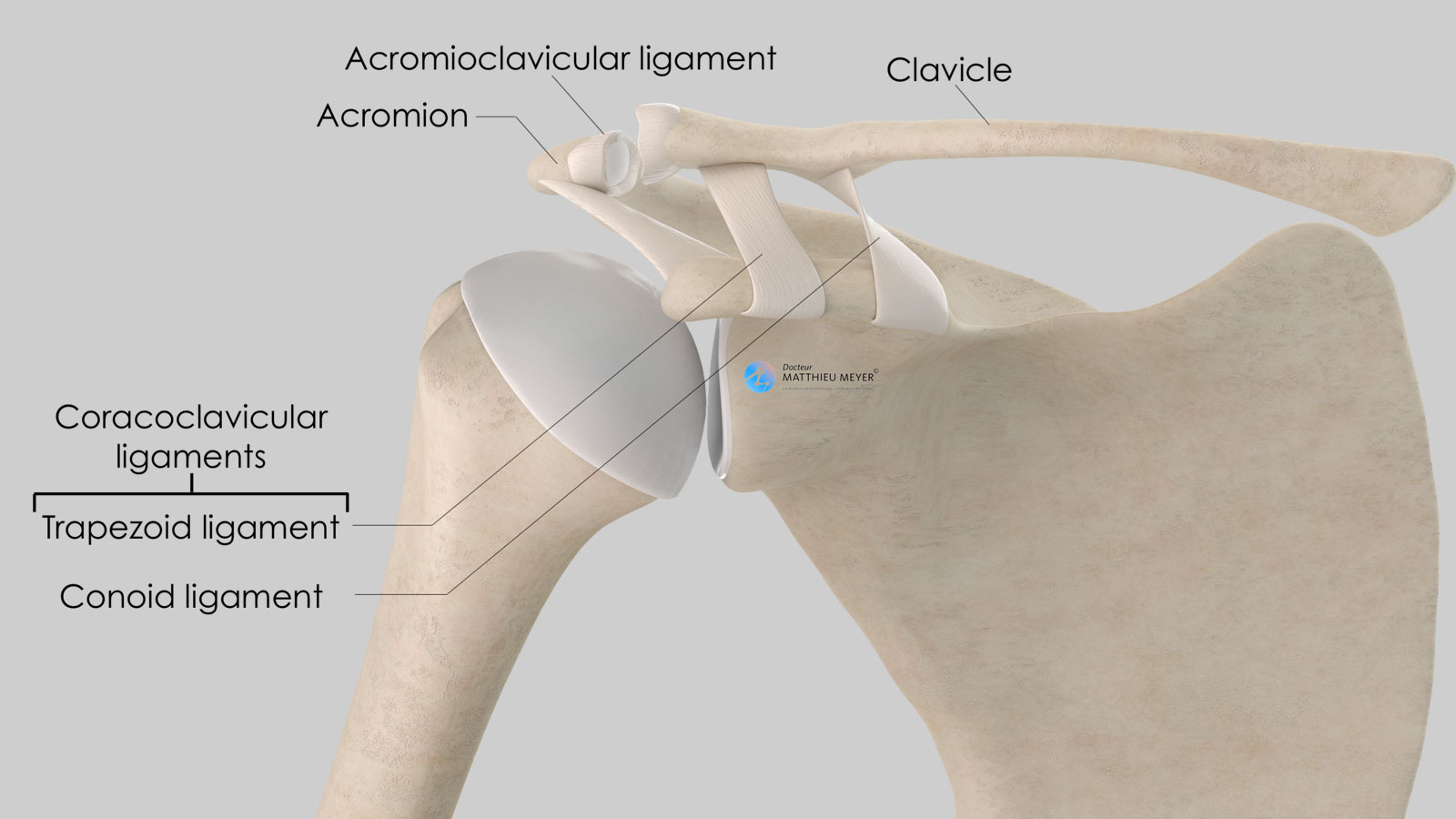
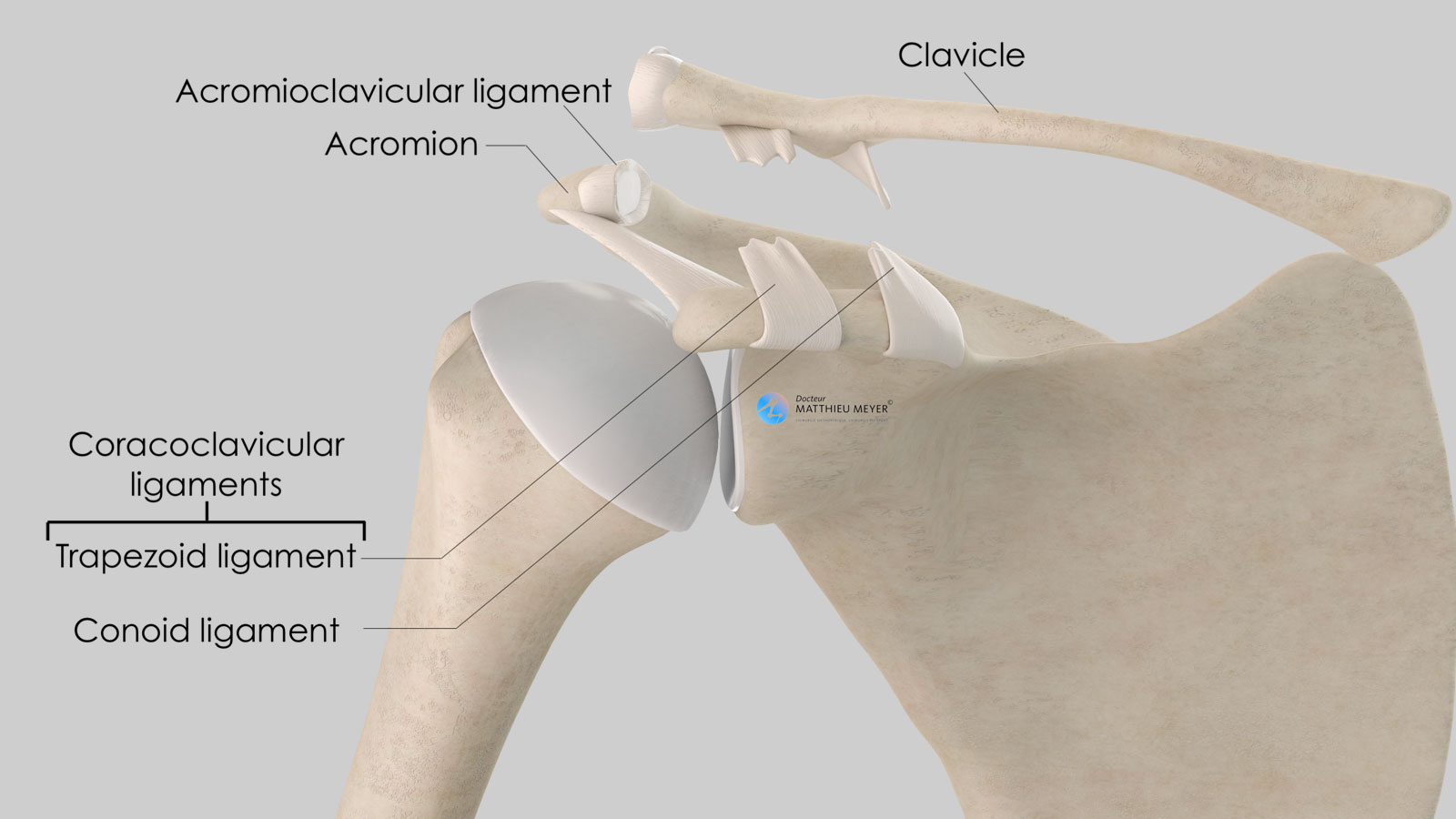
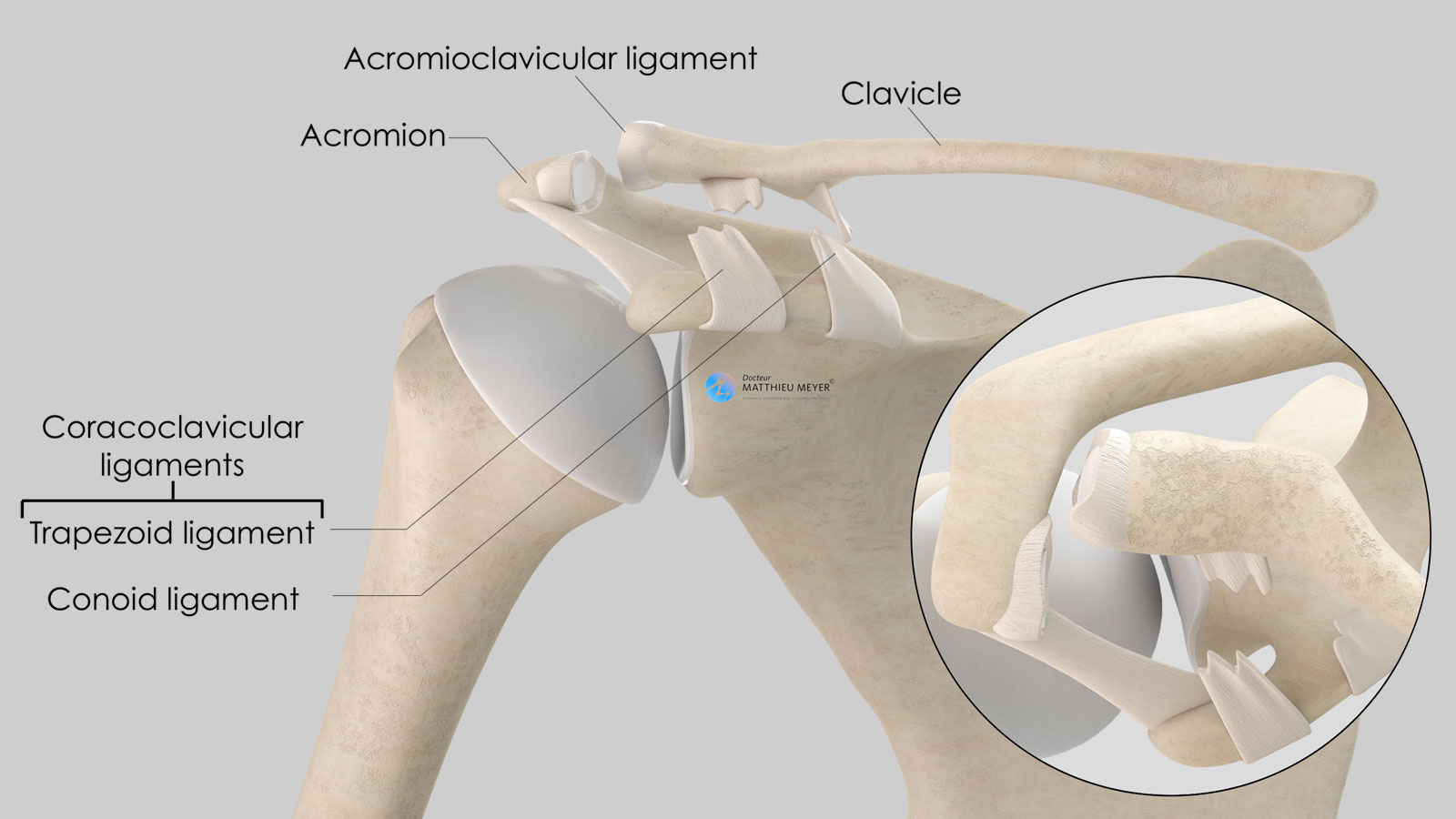
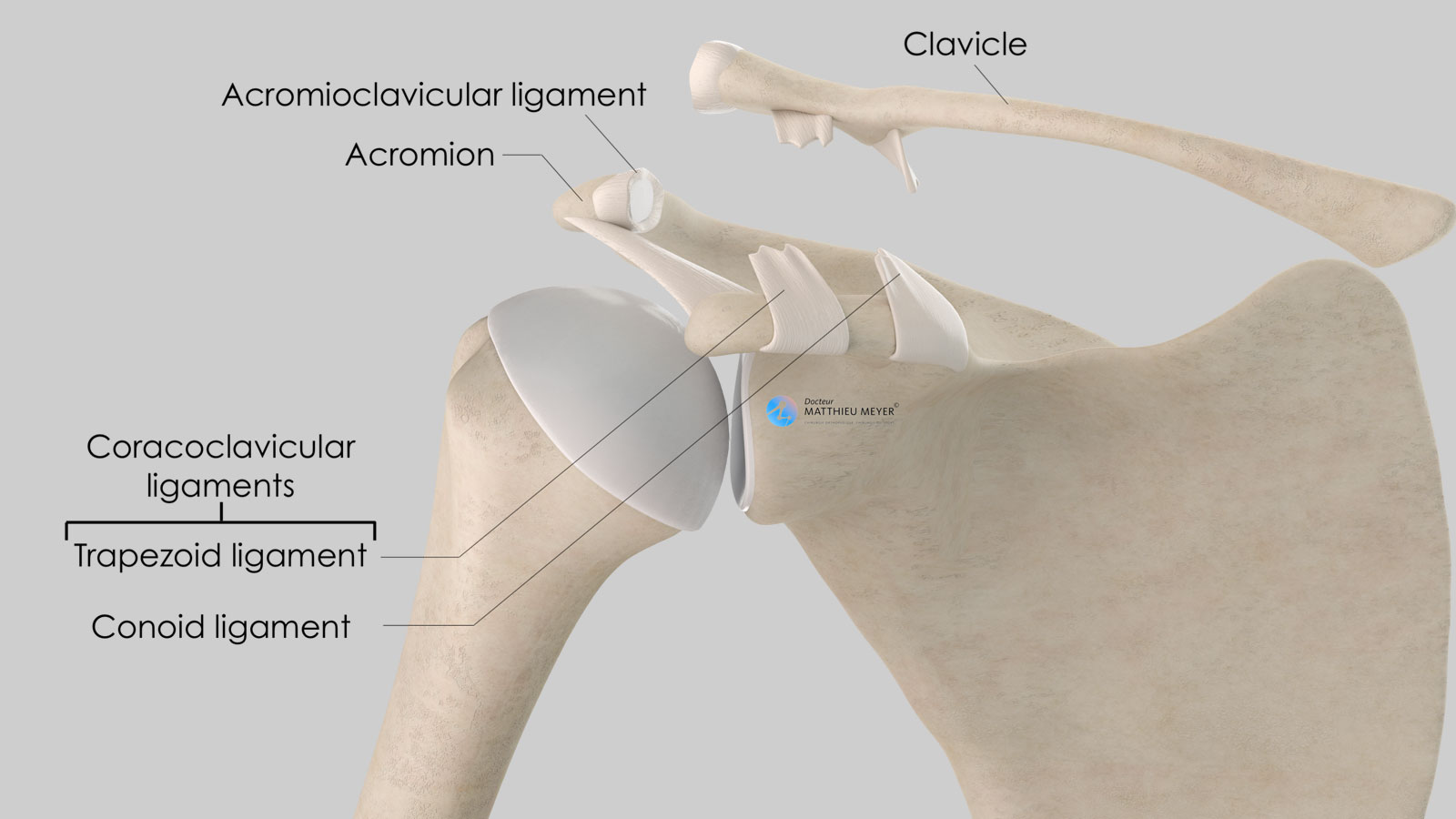
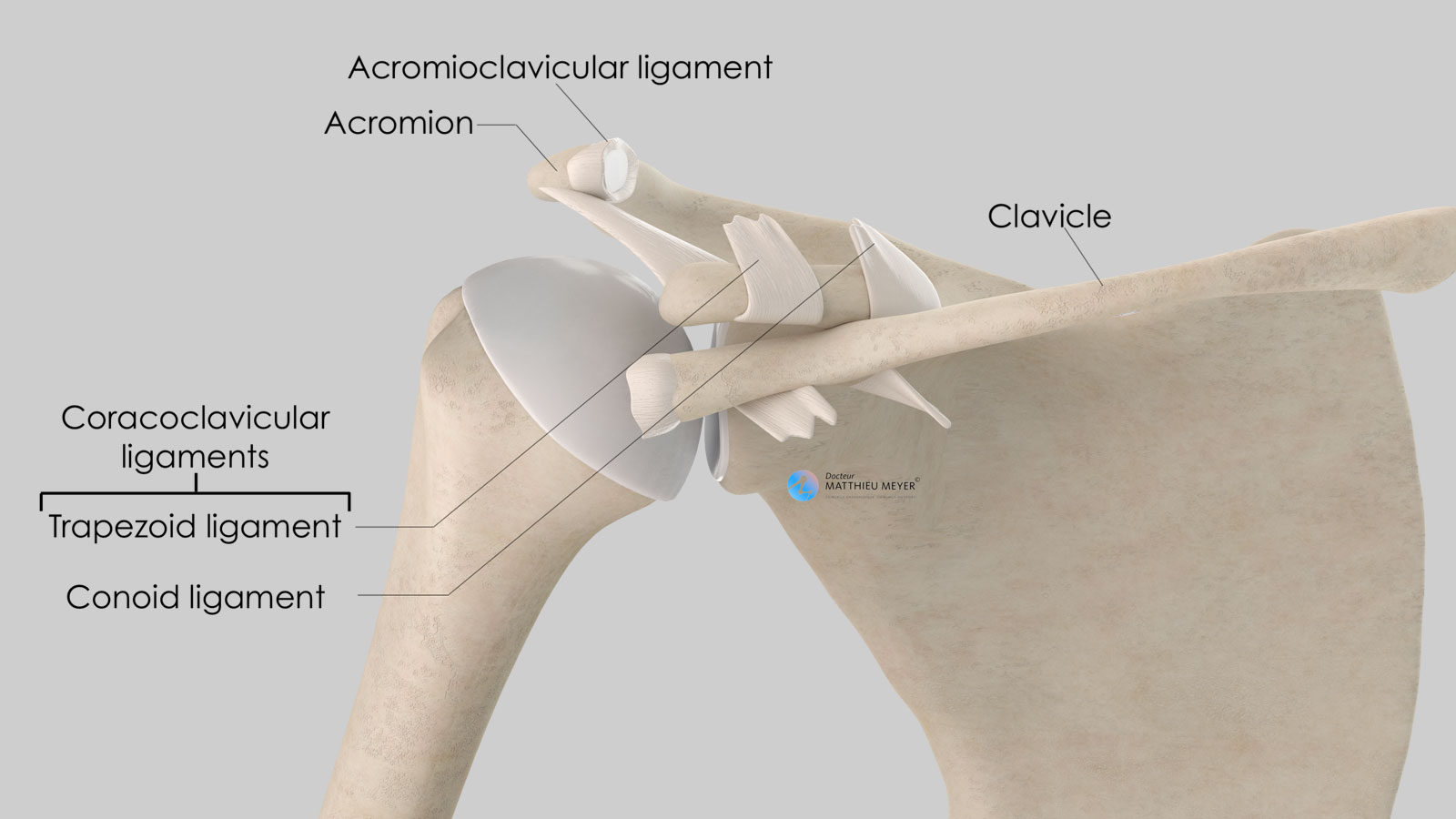
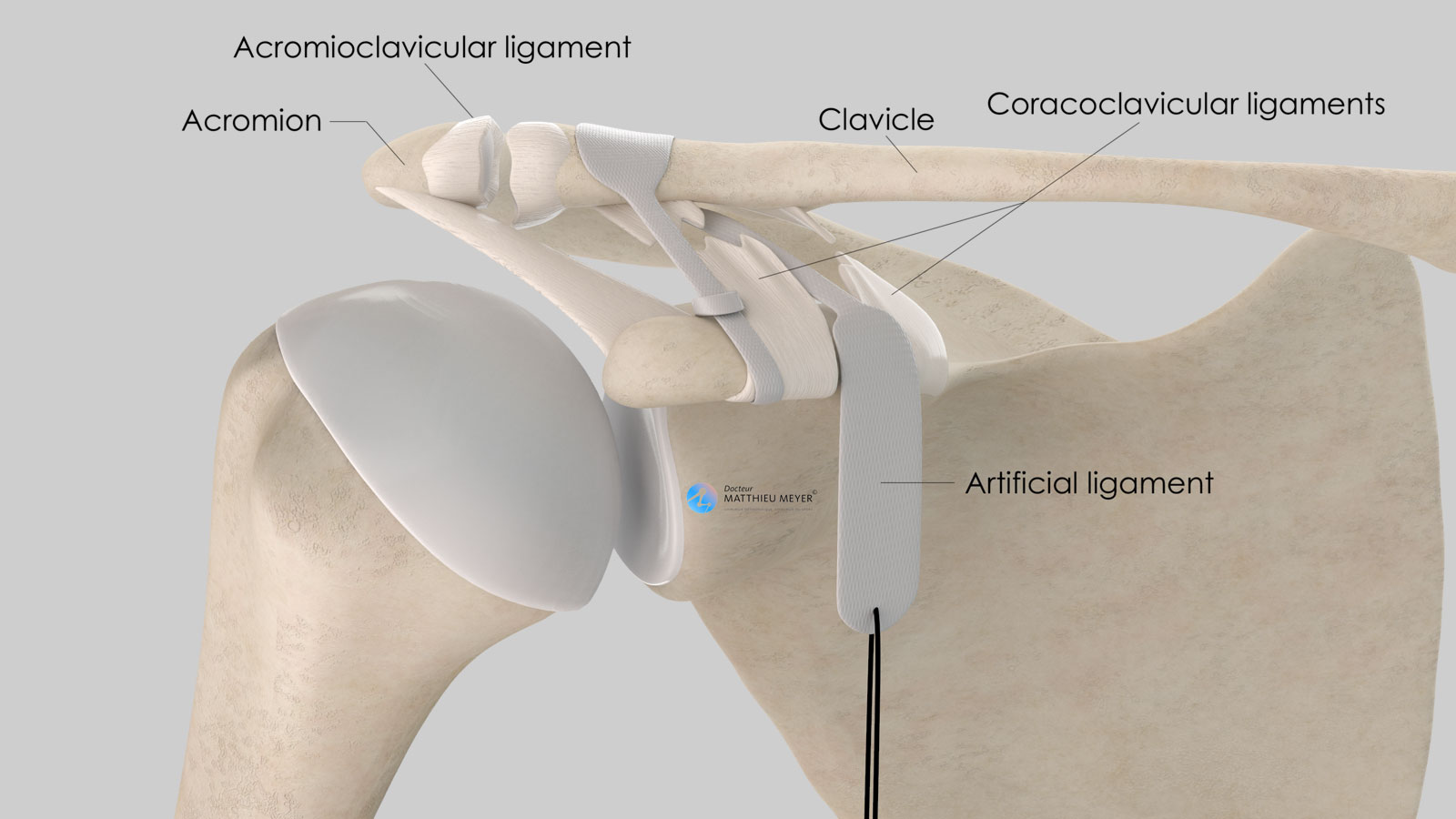
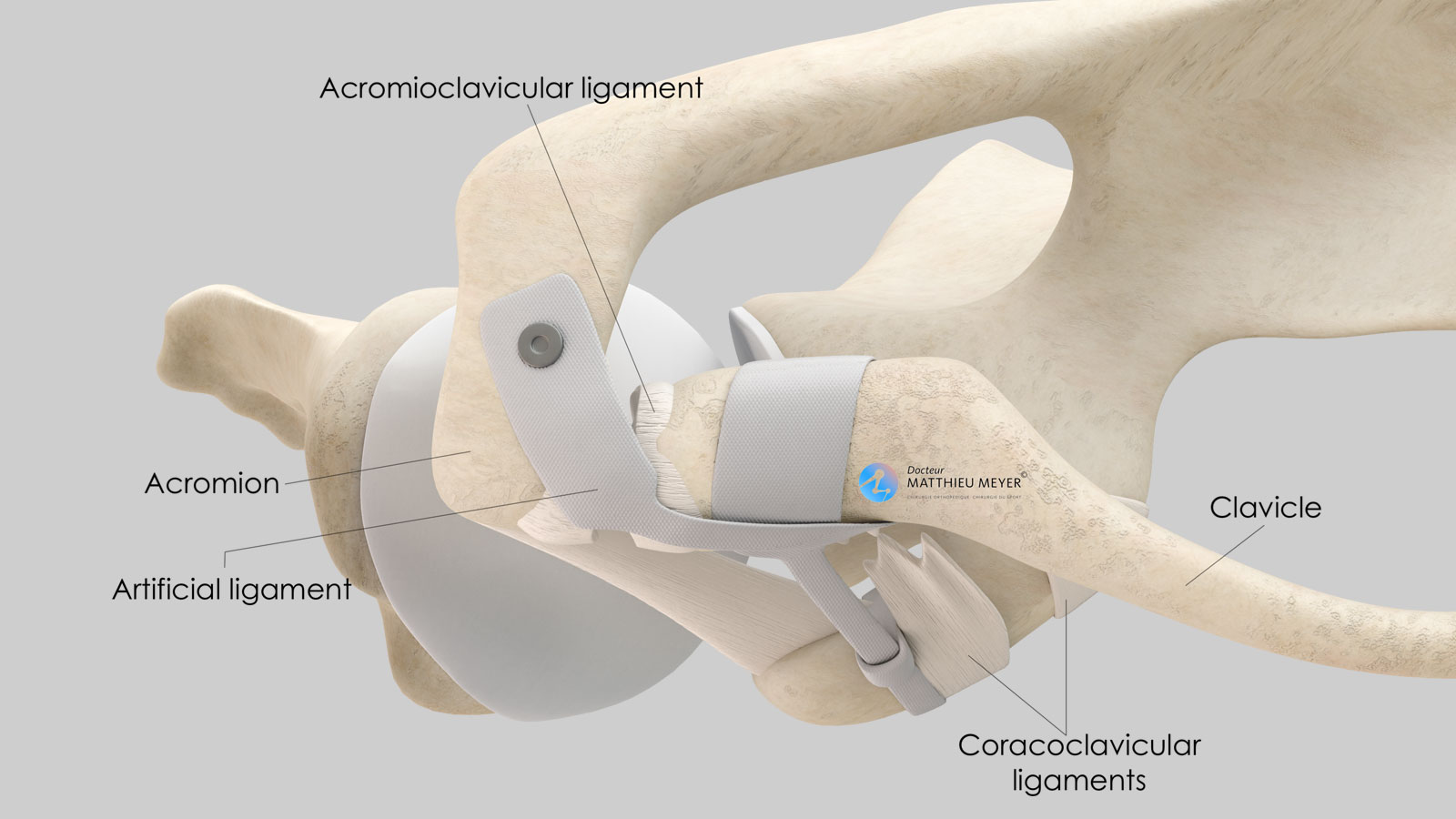
The scapula is a flat, very mobile bone that slides over the posterior part of the rib cage to which it is attached with muscles thus increasing arm range of motion. The clavicle is attached to one end of the scapula called the acromion. This acromioclavicular joint, not very mobile, is stabilised by 3 ligaments:
- The acromioclavicular ligament connecting the lateral end of the clavicle to the acromion
- The two coracoclavicular ligaments (conoid and trapezoid) connecting the coracoid, located on the anterior side of the scapula and the lateral quarter of the clavicle.
Acromioclavicular dislocation is most frequently caused by a fall on the shoulder causing the scapula, very mobile, to drop down while the clavicle, not very mobile, remains in place as it is solidly attached to the sternum.
It is therefore not surprising that these acromioclavicular dislocations are often caused by sports traumas following contact with or a fall on the lateral part of the shoulder.
Classification of acromioclavicular dislocations
After a fall on the lateral side of the shoulder, the scapula drops down causing ligament damage, firstly to the acromioclavicular ligament then the coracoclavicular ligaments. A violent trauma can result in damage to the trapezius-deltoid muscle fascia.
The Rockwood classification is the most commonly used and is based on the ligament and muscular damage caused by the trauma.
Type 3
The acromioclavicular and coracoclavicular ligaments are torn. As the scapula is no longer retained by the clavicle, it is pulled down by the weight of the arm. A characteristic protrusion of the end of clavicle appears. At this stage, the dislocation can be reduced by pushing the scapula back into its position. To do this, upward pressure is exerted on the arm under the elbow.
What examinations are necessary?
Plain x-rays are the best choice for additional examinations and show the increase in the acromioclavicular distance. More sophisticated imaging techniques such as a CT-scan or MRI are rarely necessary.
What treatments are available?
Non-surgical treatment
This combines applying an ice pack with analgesics and anti-inflammatories to limit the pain. It can be useful to wear a sling for a few days to take the weight of the arm off the shoulder.
Surgical treatment
Many types of surgery have been described using both conventional open and arthroscopic techniques.
Surgery aims to reduce and stabilise the dislocation. When the operation is carried out early, it is also preferable to achieve healing of the torn ligaments.
Arthroscopic techniques are minimally invasive resulting in minimal scarring. However, unless combined with inserting a pin or acromioclavicular tape repair, which is harmful to the cartilage in this joint, the total reduction of the dislocation is not possible as these techniques leave an anterior drawer. They can also result in a higher rate of loss of correction and some of these techniques can be complicated by a fracture of the external quarter of the clavicle.
For several years, I have preferred stabilisation using an artificial ligament Acrolig®, which has the advantage of very strongly maintaining the reduction of the coracoclavicular diastasis and the anterior acromioclavicular drawer without harming the cartilage. With a recent dislocation, the ligaments can also be sutured. The efficacy of this technique is proven, especially for numerous professional rugby players and judokas.
When is surgery necessary?
Only types 4, 5 and 6 require surgery due to the incarceration of the clavicle and trapezius-deltoid muscle damage.
It is also widely accepted that no operation is required for types 1 and 2, which do not result in a shoulder deformity and for which the results of non-surgical treatment are excellent.
However, there is no consensus for type 3 dislocations. For patients not in pain and with no considerable physical requirements, non-surgical treatment produces good results. Conversely, for young patients as well as athletes, early surgical stabilisation is preferred to restore shoulder function and anatomy as well as to relieve any pain.
What are the consequences in the absence of surgery?
Surgery is generally not required for Rockwood types 1, 2 and 3.
The progression of types 1 and 2 is excellent in most cases. Residual pain due to osteoarthritic deterioration of the acromioclavicular joint can occur in the long term but is rare.
For type 3, a potentially unsightly shoulder deformity can remain, which is even more visible in slim patients. Abnormal movements with acromioclavicular clicking or a jerking sensation can be observed. With time, osteoarthritis of the acromioclavicular joint can develop, possibly causing pain.
The operation
Before the operation
Before the operation, a pre-anaesthesia consultation, and possibly a pre-operative assessment, is conducted to check the patient is physically apt to undergo the operation and minimise the risk of postoperative complications.
The operation
The operation takes place in an operating theatre in compliance with strict standards of cleanliness and safety. The patient is placed in beach chair position on an operating table. The operation lasts about 1 hour and is carried out under general anaesthesia. It is often combined with an interscalene nerve block, an additional anaesthetic which numbs the shoulder and arm for several hours and limits postoperative pain.
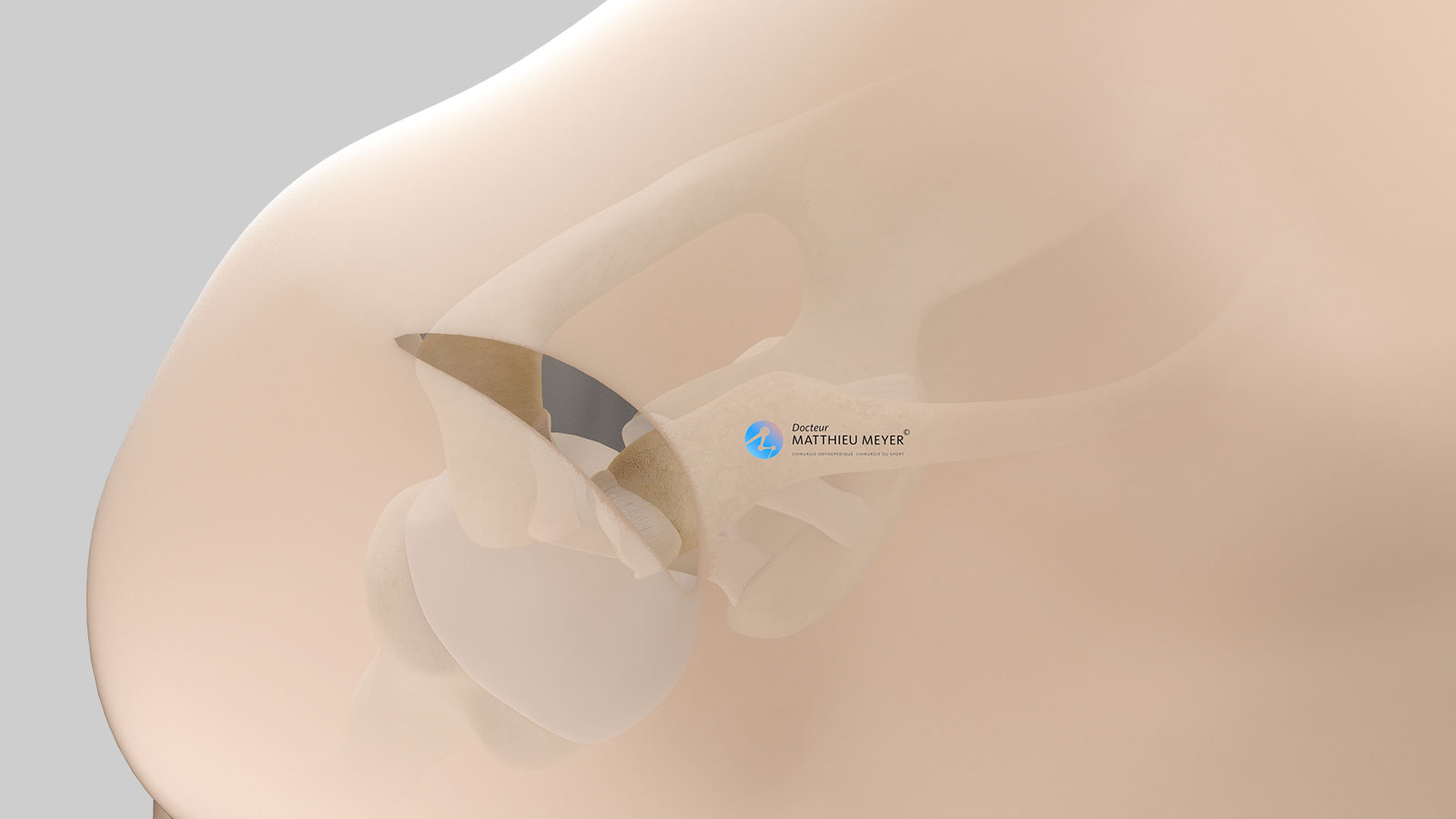
A longitudinal incision approximately 6 to 7 centimetres long is made on the superior side of the shoulder.
The acromioclavicular dislocation is reduced and held in place with an artificial ligament Acrolig®.
For recent dislocations, the coracoclavicular ligaments are sutured and any damage to the trapezius-deltoid fascia is repaired.
For old dislocations, if the cartilage on the acromioclavicular joint is involved causing pain, the lateral quarter of the clavicle is resected during the operation.
At the end of the procedure, a suction drain can be inserted in the incision to prevent the formation of hematoma.
After the operation
The shoulder is numbed with an interscalene block for 12 to 18 hours. Medication and ice also provide effective postoperative pain management.
The surgery can be performed as an outpatient procedure (leave hospital the day of the operation) or a short stay. The patient can return home when discharged.
The shoulder is kept in an orthopaedic sling for 6 weeks. There will be no rehabilitation during this period to ensure the reduction does not fail during the healing phase as the strain exerted is very considerable.
When the patient is discharged from the clinic, a consultation with follow-up x-rays is scheduled with the surgeon 4 to 6 weeks after the operation to check the acromioclavicular reduction is still in place and that there are no complications. A second check-up is generally recommended approximately 3 months after the operation.
The duration of medical leaves depends on the patient’s profession but generally varies between 1½ and 2 months. It is longer for manual work.
Driving can be resumed 2 months after the operation.
Sports can be resumed using the shoulder operated on approximately 3 to 4 months after the operation.
Risks linked to the operation
Unfortunately, zero risk does not exist in surgery. Any operation has its risks and limitations, which you must accept or not undergo the operation. However, if an operation is proposed, the surgeon and the anaesthetist consider that the expected benefits far outweigh the risk incurred.
Some risks, such as microbial infections of the surgical site, are common to all types of surgery. Fortunately, this complication is rare but when it occurs requires another operation and a course of antibiotics. Bruising can also appear around the surgical site. This is usually prevented or reduced with a suction drain inserted at the end of the operation and removed in the days following the operation. However, in the case of severe bleeding during or following the operation, another operation to stop the haemorrhage or a blood transfusion may be required.
Blood clots can form in the veins in the arm (thrombophlebitis) or lungs (pulmonary embolism). If the anaesthetist considers the risk high, you may be given a treatment to prevent this.
In rare cases, the shoulder remains stiff, hot, and painful for several months after the operation. This complication, known as algodystrophy or Chronic Regional Pain Syndrome (CRPS), is unpredictable and sometimes takes a long time to heal.
Finally, rarer complications can also occur. Blood vessels (arteries, veins) can be accidentally damaged and will require vascular surgery (bypass). Nerves can also be damaged accidentally during the operation with a risk of paralysis or loss of feeling in the limb operated on, which can be transitory or permanent.
Finally, a slight loss of acromioclavicular reduction may be observed, generally with no functional consequences.
If you have any concerns about the operation, do not hesitate to talk to your surgeon or the anaesthetist and they will answer any questions you may have.
In summary...
When is surgery necessary?
In the case of type 4, 5 and 6 acromioclavicular dislocation and type 3 in young subjects or athletes
Aim of the operation
Reduction and stabilisation of the acromioclavicular dislocation
Which anaesthesia?
General
Duration of hospitalisation
Outpatient or short stay (1 night)
Postoperative immobilisation
Orthopaedic sling for 6 weeks
Duration of rehabilitation
1 to 3 months
Duration of medical leave
6 to 8 weeks in the case of sedentary work, longer for manual work
Resumption of car driving
2 months after the operation
Resumption of sport
3 to 4 months after the operation
Make an appointment
please do not hesitate to contact us or make an appointment online via DoctoLib