Revision Total Hip Replacement
Home » Operations » Hip Surgery » Total Hip Replacement » Revision Total Hip Replacement
What is the problem?
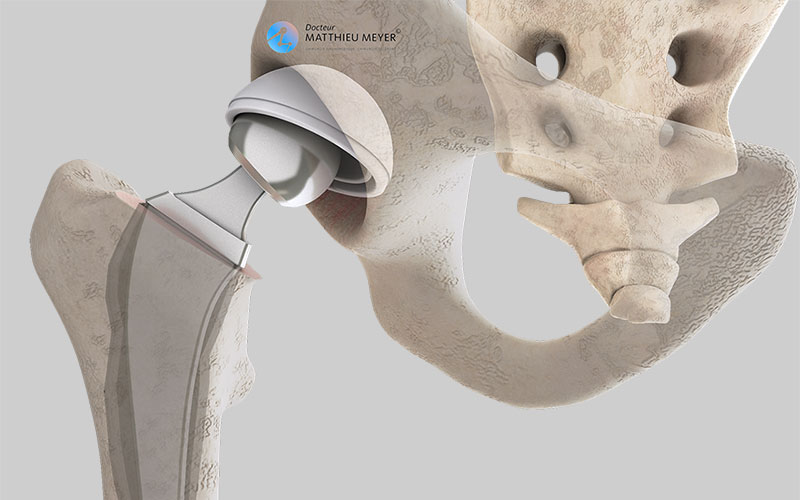
A hip prosthesis comprises two parts called implants: an acetabular component attached to the pelvis and a femoral stem attached to the femur. Over time, the rubbing around the area of contact between the 2 implants can result in the deterioration of the prosthesis, especially the acetabular component when it is made of plastic (polyethene). Extreme wear can result in abnormal contact between the implants and may also cause resorption of the bone in contact with the prosthesis thus resulting in one or even both of the implants loosening. When the prosthesis becomes loose, the hip becomes very painful when moving and putting weight on the leg. Consequently, all or part of the prosthesis needs to be replaced.
More rarely, it is necessary to change the prosthesis for other reasons: recurrent dislocations, painful rubbing of a tendon on part of the prosthesis, badly tolerated unequal leg length linked to the prosthesis.
Before the operation
A revision hip replacement requires an operation and the type of prosthesis best suited to the patient is chosen during pre-surgical consultations. A pre-anaesthesia consultation and a preoperative assessment are conducted to check the patient is physically apt to undergo the operation and minimise the risk of postoperative complications, especially infections. This assessment generally includes a blood test, a cardiovascular check-up, as well as a dental check-up and a urine test to ensure there are no infections and thus avoid any microbial contamination of the prosthesis.
The different types of revision hip replacement
Depending on which parts are worn or loose, the surgeon determines which of the following the patient requires:
- Replacement of the acetabular implant
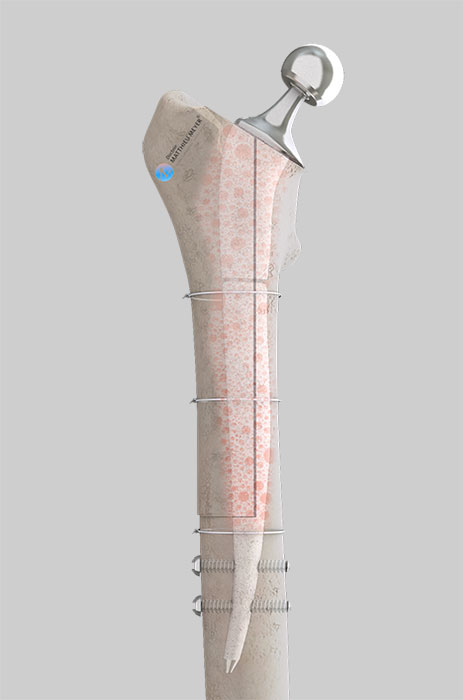
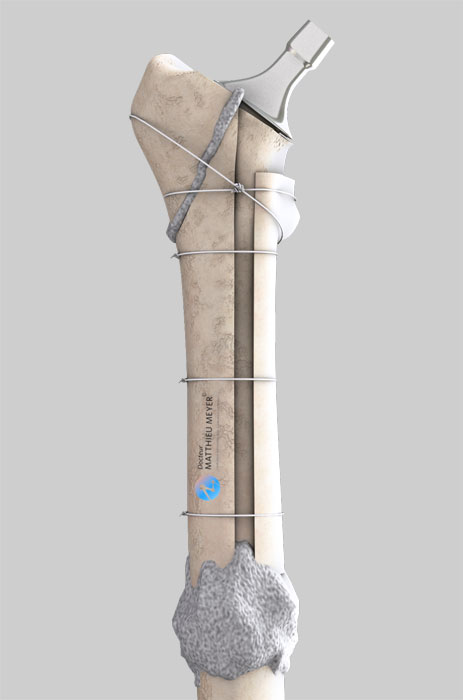
- Replacement of the femoral stem
- Replacement of both implants
A femoral osteotomy (segmentation of the bone) may be required to remove the femoral stem. In this case, the femur must then be reduced and held in place with wires or a plate.
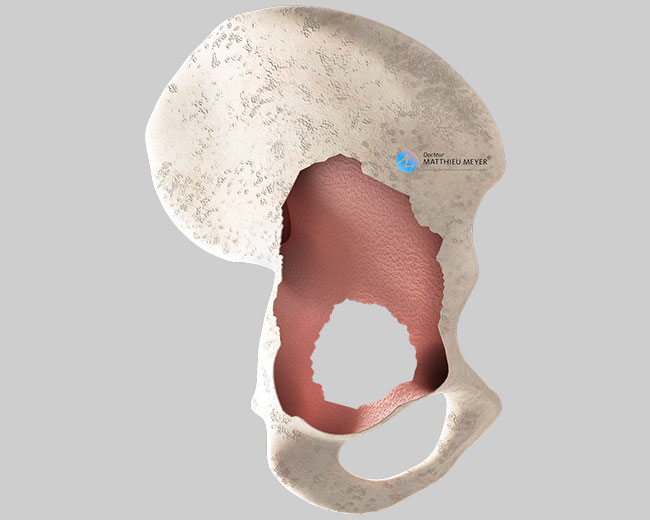
Sometimes, a bone graft may be required in the case of significant bone loss around the implants and is incorporated in the recipient bone. In most cases, the bone is taken from the femoral heads of selected patients (after questioning and serological tests) who have had a total hip replacement. This bone is treated to inactivate any residual microbes or viruses and then frozen until use. Contrary to an organ transplant, a bone graft does not require anti-rejection medication.
Finally, destruction of the acetabular bone may require the incorporation of a wire mesh in addition to a bone graft to attach the new acetabular implant.
The operation
The duration of the operation varies according to the number of implants to be changed and the deterioration of the bone. It generally lasts between 1.5 and 3 hours but can sometimes be longer. This operation can be carried out under general or spinal anaesthetic. The latter is a regional anaesthetic anaesthetising the lower part of the body (as with an epidural). The anaesthetist will decide on the most suitable anaesthetic together with the patient.
From a technical point of view, the surgeon will follow the incision made for the primary hip replacement, which may need to be extended to carry out the procedure. It is not recommended to create a new “route” to the joint if one has already been used. However, it is sometimes necessary to change the approach if the approach used previously is not suitable for all the surgical procedures required.
After the operation
Rehabilitation begins the day after the operation with the help of physiotherapists. Weight-bearing on the limb operated on again depends on what happened during the operation. It can be immediate or delayed for several weeks in the case of bone reconstruction. Crutches are used to start with but are gradually abandoned.
The stay in hospital is often between 4 and 8 days. When leaving the clinic, the patient can return home as long as it is not too difficult to access and they have someone to help with daily activities (shopping, meals…). Otherwise, a stay of approximately 1 month at a rehabilitation centre can be considered.
When the patient is discharged from the clinic, a consultation with follow-up x-rays of the implant is scheduled with the surgeon, generally 4 to 6 weeks after the operation, to ensure the patient is making satisfactory progress. The frequency of the subsequent checkups is determined by the surgeon. Once recovery is satisfactory, x-rays of the prosthesis are then recommended every 2 years to ensure there is no abnormal wear of the implants or the surrounding bone.
Risks linked to the operation
Unfortunately, zero risk does not exist in surgery. Any operation has its risks and limitations, which you must accept or not undergo the operation. However, if an operation is proposed, the surgeon and the anaesthetist consider that the expected benefits clearly outweigh the risk incurred.
Some risks, such as microbial infections of the surgical site, are common to all types of surgery. Fortunately, this complication is rare but when it occurs requires the lavage of the prosthesis during another procedure and a course of antibiotics. More rarely, some infections can require the prosthesis to be replaced. Bruising can also appear around the surgical site. This is usually prevented or reduced with a suction drain inserted at the end of the operation and removed in the days following the operation. Exceptionally, a procedure may be required to reduce the pressure with severe bruising and in the case of severe bleeding, a blood transfusion may sometimes be necessary.
Hip surgery also increases the risk of phlebitis, which can lead to a pulmonary embolism. To minimise this risk, blood thinners (in the form of daily injections or tablets) are prescribed for the entire month following the operation.
There are also risks specific to hip replacement surgery. Firstly, dislocation of the prosthesis is possible. Dislocation most often occurs in the first weeks following the hip replacement when everything around it is not yet fully healed. When dislocated, a mild anaesthetic is necessary to put it back into place. It is also possible that the two legs are not the same length after the operation. This limb-length discrepancy is often well tolerated and goes unnoticed. If this is not the case and there is a limp, an insole may be prescribed.
Finally, rarer complications can also occur. A fracture of the femur can occur during the procedure, which generally delays the resumption of weight-bearing. Nerves can also be damaged accidentally during the operation with a risk of paralysis or loss of feeling in the limb operated on, which can be transitory or permanent.
If you have any concerns about the operation, do not hesitate to talk to your surgeon or the anaesthetist and they will answer any questions you may have.
A few questions about revision hip replacements
What is the expected outcome of a revision hip replacement?
A revision hip replacement is required when the prosthesis in place no longer provides satisfactory results. It can be painful, dislocate frequently or cause badly tolerated unequal leg length. The aim of the operation is to achieve functional improvement and thus the most satisfactory quality of life possible. However, the result is not always as satisfactory as with a primary hip replacement due to the complexity of this type of operation.
What is the lifespan of the new hip prosthesis?
It is not possible to give an accurate lifespan for the new prosthesis as too many factors are involved including bone quality around the implant, the bearing surfaces, or possible history of revision surgery on the same hip.
All we can say is that generally speaking, the lifespan of a new prosthesis is often shorter than that of the previous prosthesis.
Are there any movements that should be avoided after a revision hip replacement?
Yes, after a revision hip replacement, you must be careful for at least 2 months to avoid dislocation of the prosthesis. Consequently, you must avoid bending too far and crossing your legs.
Do I need to make any changes at home after a revision hip replacement?
No definitive changes are necessary. However, during the post-operative period, ground-floor accommodation is best if possible. You should avoid using low seats and a raised toilet seat is more comfortable.
Where will the scar be?
Generally, the old scar is used. However, it is sometimes necessary to extend it to make it easier to change the prosthesis. In some cases, another approach is required which your surgeon will tell you about during the preoperative consultation.
Do I have to be totally unconscious during the operation?
No, this operation can be performed under regional anaesthesia if there are no contra-indications.
How long is the stay in hospital?
The length of stay generally varies between 4 and 8 days.
When can I drive after the operation? Can I travel by car?
It depends on the type of revision. Before driving again, you must be fully fit and capable of stopping in an emergency. A minimum of 4 weeks is necessary before driving again, but most of the time it is better to wait 2 months. As a passenger, you have to wait at least 2 weeks and avoid cars with low seats until the 2nd month after the operation.
How long will I be off work after the operation?
It depends on your profession and the level of physical activity required but generally varies between 2 and 3 months.
Can I do any sport after a revision hip replacement?
Yes, but only sports that put little strain on the hip. Swimming and cycling are therefore best. You generally have to wait until the 6th month after the operation before resuming sport.
What are the risks linked to revision hip replacement surgery?
Unfortunately, zero risk does not exist in surgery. Any operation has its risks and limitations, which you must accept or not undergo the operation. However, if an operation is proposed, the surgeon and the anaesthetist consider that the expected benefits far outweigh the risk incurred.
Some risks, such as microbial infections of the surgical site, are common to all types of surgery. Fortunately, this complication is rare but when it occurs requires the lavage of the prosthesis during another procedure and a course of antibiotics. More rarely, some infections can require the prosthesis to be replaced. Bruising can also appear around the surgical site. This is usually prevented or reduced with a suction drain inserted at the end of the operation and removed in the days following the operation. Exceptionally, a procedure may be required to reduce the pressure with severe bruising and in the case of severe bleeding, a blood transfusion may sometimes be necessary.
Hip surgery also increases the risk of phlebitis, which can lead to a pulmonary embolism. To minimise this risk, blood thinners (in the form of daily injections or tablets) are prescribed for the entire month following the operation.
There are also risks specific to hip replacement surgery. Firstly, dislocation of the prosthesis is possible. Dislocation most often occurs in the first weeks following the hip replacement when everything around it is not yet fully healed. When dislocated, a mild anaesthetic is necessary to put it back into place. It is also possible that the two legs are not the same length after the operation. This limb-length discrepancy is often well tolerated and goes unnoticed. If this is not the case and there is a limp, an insole may be prescribed.
Finally, rarer complications can also occur. A fracture of the femur can occur during the procedure, which generally delays the resumption of weight-bearing. Nerves can also be damaged accidentally during the operation with a risk of paralysis or loss of feeling in the limb operated on, which can be transitory or permanent.
If you have any concerns about the operation, do not hesitate to talk to your surgeon or the anaesthetist and they will answer any questions you may have.
In summary...
When is surgery necessary?
If the implant is worn, painful, or frequently dislocates
Aim of the operation
Functional improvement
Which anaesthesia?
General or regional determined during the pre-operative anaesthesia consultation
Length of stay
Between 4 and 8 days
Resumption of weight-bearing
Immediate or delayed several weeks according to the bone surgery carried out during the operation
After the operation
Return home if help at home and not many stairs, otherwise discuss stay at rehabilitation centre
Duration of rehabilitation
Generally 2 months
Duration of medical leave
2 to 3 months
Resumption of car driving
At least 1 month after the operation, often 2 months
Resumption of sport
6 months after the operation but only low-impact sports
Make an appointment
please do not hesitate to contact us or make an appointment online via DoctoLib