Anterior Hip Impingement Arthroscopy
Home » Operations » Hip Surgery » Anterior Hip Impingement » Anterior Hip Impingement Arthroscopy
What is the problem?
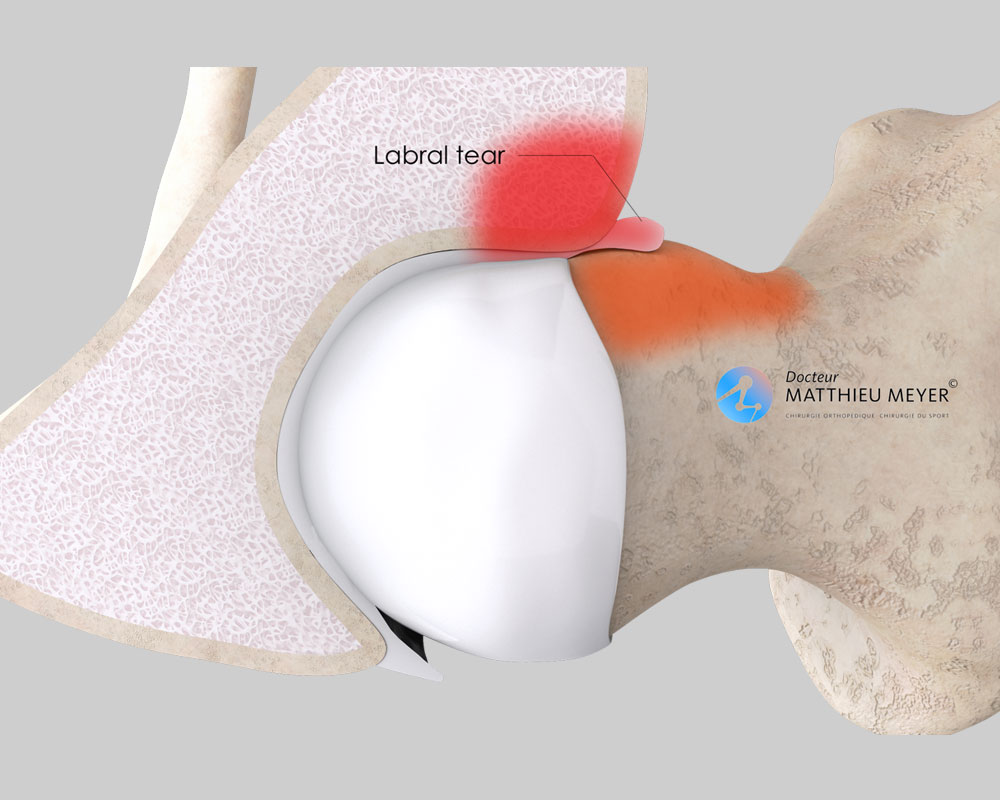
The hip is the joint between the socket in the pelvis called the acetabulum and the femoral head, and like all joints, it is covered with cartilage enabling the femoral head to slide in the acetabulum freely and painlessly. Around the entire circumference of the acetabulum is a “seal” called the labrum, which increases joint stability and helps prevent dislocations. It also plays a role of shock absorber when weight-bearing.
Abnormal contact between the femoral neck and the edge of the acetabulum causes anterior hip impingement. Two types of deformation, which are sometimes combined, can contribute to this abnormal contact:
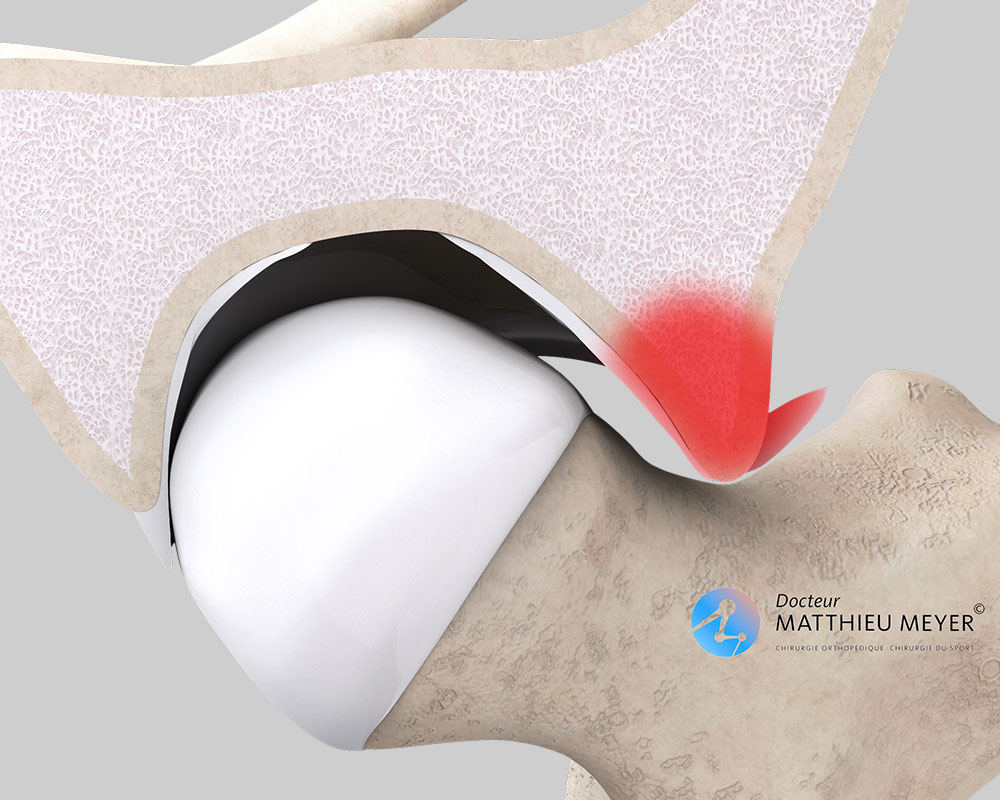
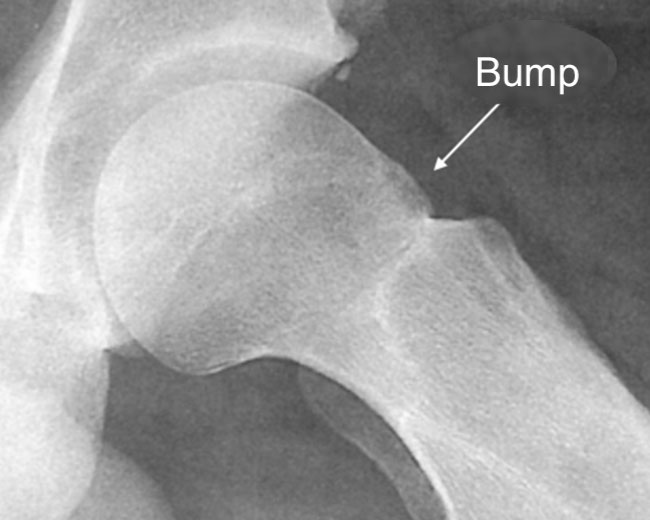
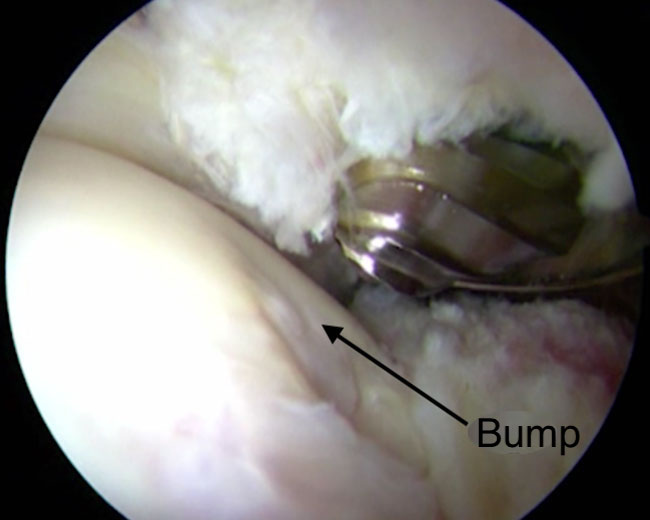
- A bump on the anterior part of the femoral neck results in premature contact with the edge of the acetabulum during bending of the hip thus damaging the anterior labrum. This is known as cam impingement.
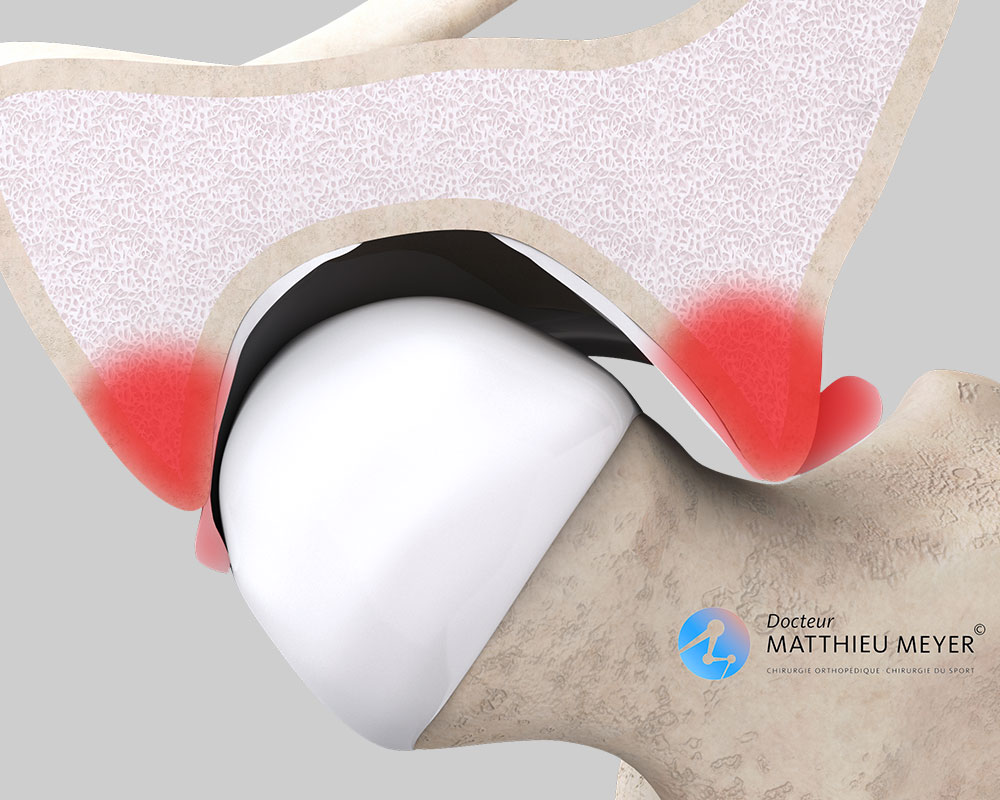
- Excessive coverage of the anterior edge of the acetabulum that extends too low impinging on the femoral neck during hip flexion causing damage to the anterior labrum and decoaptation of the joint which damages the posterior labrum. This is known as pincer impingement.
Anterior hip impingement is primarily observed in patients who participate in activities involving repeated hip flexion such as dancing, martial arts, or climbing. It initially causes pain in the groin during sports activities. With time, the pain can become increasingly constant and is accompanied by a decrease in hip mobility.
How is the diagnosis confirmed?
First and foremost, hip x-rays are conducted to identify any anomalies that may contribute to the impingement (bump on the femoral neck, excessive coverage of anterior acetabulum). The x-rays will also help eliminate any other causes of hip pain such as osteoarthritis or necrosis of the femoral head.
When anterior hip impingement is strongly suspected, an MRI or CT arthrogram of the hip must be prescribed. These examinations help highlight the presence of damage to the labrum or cartilage linked to anterior impingement and determine the nature of the surgical procedure to be carried out.
What treatments are available?
Non-surgical treatment
This involves stopping the sports activities causing the pain. Medication to decrease the pain (analgesics, anti-inflammatories) can be prescribed. Finally, anti-inflammatory cortisone injections in the hip joint can be carried out. As the hip is a deep joint, the injections are systematically x-ray or ultrasound guided.
The medical treatment aims primarily to eliminate the pain without treating the cause. It is effective but the pain often flares up when sport is resumed.
Surgical treatment: hip arthroscopy
The aim is to relieve the pain by flattening the area of contact between the femoral neck and the edge of the acetabulum, as well as to repair, whenever possible, the acetabular labrum and thus reduce the risk of cartilage damage (osteoarthritis).
When is surgery necessary?
A hip arthroscopy must be performed before the damage to the cartilage becomes too serious (osteoarthritis), as an arthroscopy is ineffective in relieving the pain once osteoarthritis sets in.
What will happen in the absence of treatment?
In the absence of treatment, the repeated contact between the femoral neck and the edge of the acetabulum will lead to the progressive deterioration of the labrum then the cartilage, which can result in hip osteoarthritis after a few years.
The operation
The operation takes place in an operating theatre in compliance with strict standards of cleanliness and safety. The patient is placed supine on an orthopaedic operating table to enable traction to access the hip.
The operation lasts about 1 hour, plus the time required for the anaesthetic and positioning the patient in the operating theatre. This operation can be carried out under general or spinal anaesthesia. The latter is a regional anaesthetic anaesthetising the lower part of the body (as with an epidural). The anaesthetist will decide on the most suitable anaesthetic together with the patient.
The procedure is performed using arthroscopic surgery, a minimally invasive surgical technique that enables the operation to be carried out through small incisions 5 millimetres in length located on the anterior and lateral side of the hip. A miniaturised camera is inserted in the joint so the procedure can be followed on a screen. More rarely, the operation can be carried out through a small incision 6 centimetres in length on the anterior side of the hip.
The operation aims to remove the area of impingement.
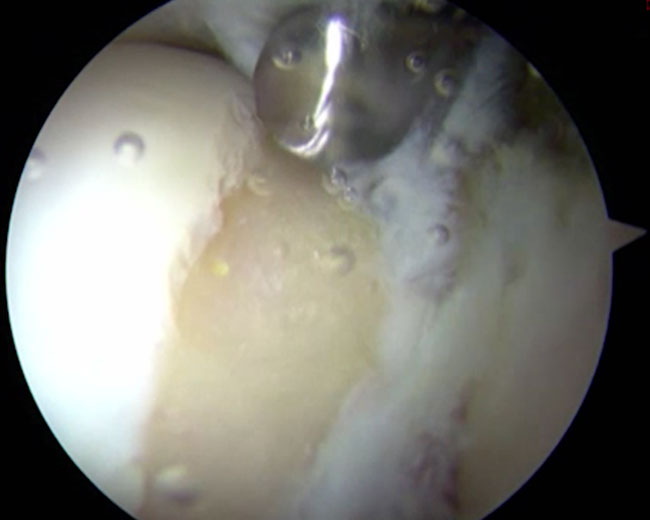
In the case of cam impingement, the bump on the femoral neck is flattened.
In the case of pincer impingement, the labrum is detached and the excess bone of the acetabulum is trimmed.
At the end of the procedure, if its condition allows, the labrum is reinserted on the acetabular edge. Otherwise, the damaged part of the labrum is removed.
After the operation
The initial pain is usually controlled with medication.
A short stay of fewer than 3 days is usually required for this operation.
For the first four weeks, a nurse will visit you at home to change the dressings and administer the anticoagulant injections.
Resumption of weight-bearing: a physiotherpatist will help you stand the day after the operation. Initially, crutches are used when walking but will be rapidly abandoned if the procedure was only performed on the femoral neck. However, if the edge of the acetabulum was trimmed, crutches must be used to relieve the strain on the hip for 3 weeks after the operation.
Post-operative rehabilitation is not usually necessary. Progressive resumption of walking is often the only rehabilitation required.
A check-up is scheduled 4 weeks after the procedure to assess recovery, detect any potential complications, as well as to adjust rehabilitation if progress is not as expected. Another check-up usually takes place in the 3rd month after the operation.
Resuming work and sport
The duration of medical leave depends on the patient’s profession and the type of operation but is generally between 1 and 3 months.
Sport can be resumed progressively from the 4th month after the operation but it is often necessary to wait 6 months to return to their previous level.
Risks linked to the operation
Unfortunately, zero risk does not exist in surgery. Any operation has its risks and limitations, which you must accept or not undergo the operation. However, if an operation is proposed, the surgeon and the anaesthetist consider that the expected benefits far outweigh the risk incurred.
Some risks, such as microbial infections of the surgical site, are common to all types of surgery. Fortunately, this complication is rare but when it occurs requires another operation and a course of antibiotics. Bruising can also appear around the surgical site. According to the extent of the bleeding, surgical drainage of the bruise or a transfusion may be necessary.
Surgery of the lower limbs also increases the risk of phlebitis, which can lead to a pulmonary embolism. To minimise this risk, blood thinners (in the form of daily injections) are prescribed for 3 weeks following the operation.
Finally, rarer nerve or vascular complications can also occur. Nerves can be damaged accidentally leading to pain, a loss of feeling, or even paralysis of some parts of the perineum or the thigh that can be transitory or permanent. In the event of accidental arterial damage, vascular surgery may be necessary.
If you have any concerns about the operation, do not hesitate to talk to your surgeon or the anaesthetist and they will answer any questions you may have.
Expected outcome
This surgery is relatively recent, so long-term results are not yet available.
The short-term results are encouraging as patients have reported improvement in 90% of cases and the possibility of resuming sports activities in 80% of cases. The outcome is better when the procedure is carried out before there is any cartilage damage (osteoarthritis).
In the event of residual pain, cortisone or hyaluronic acid injections in the hip should be discussed.
In summary...
Who should undergo surgery?
Patients with anterior hip impingement confirmed by an MRI or CT arthrogram, in the absence of severe ostoearthritic damage
Surgical technique
Arthroscopy
Which anaesthesia?
General or regional according to the patient’s history and wishes (determined with the anaesthetist)
Duration of hospitalisation
2 to 3 nights
Resumption of
weight-bearing
Immediate, alleviated with crutches (to be kept for 4 weeks if the edge of the acetabulum is trimmed)
Duration of medical leave
1 to 3 months depending on the patient’s profession
Resumption of car driving
4 weeks after the operation
Resumption of sport
Progressively from the 4th month after the operation
Make an appointment
please do not hesitate to contact us or make an appointment online via DoctoLib