Fractures of the clavicle
Home » Operations » Shoulder Surgery » Traumatic Shoulder Injuries » Fractures of the clavicle
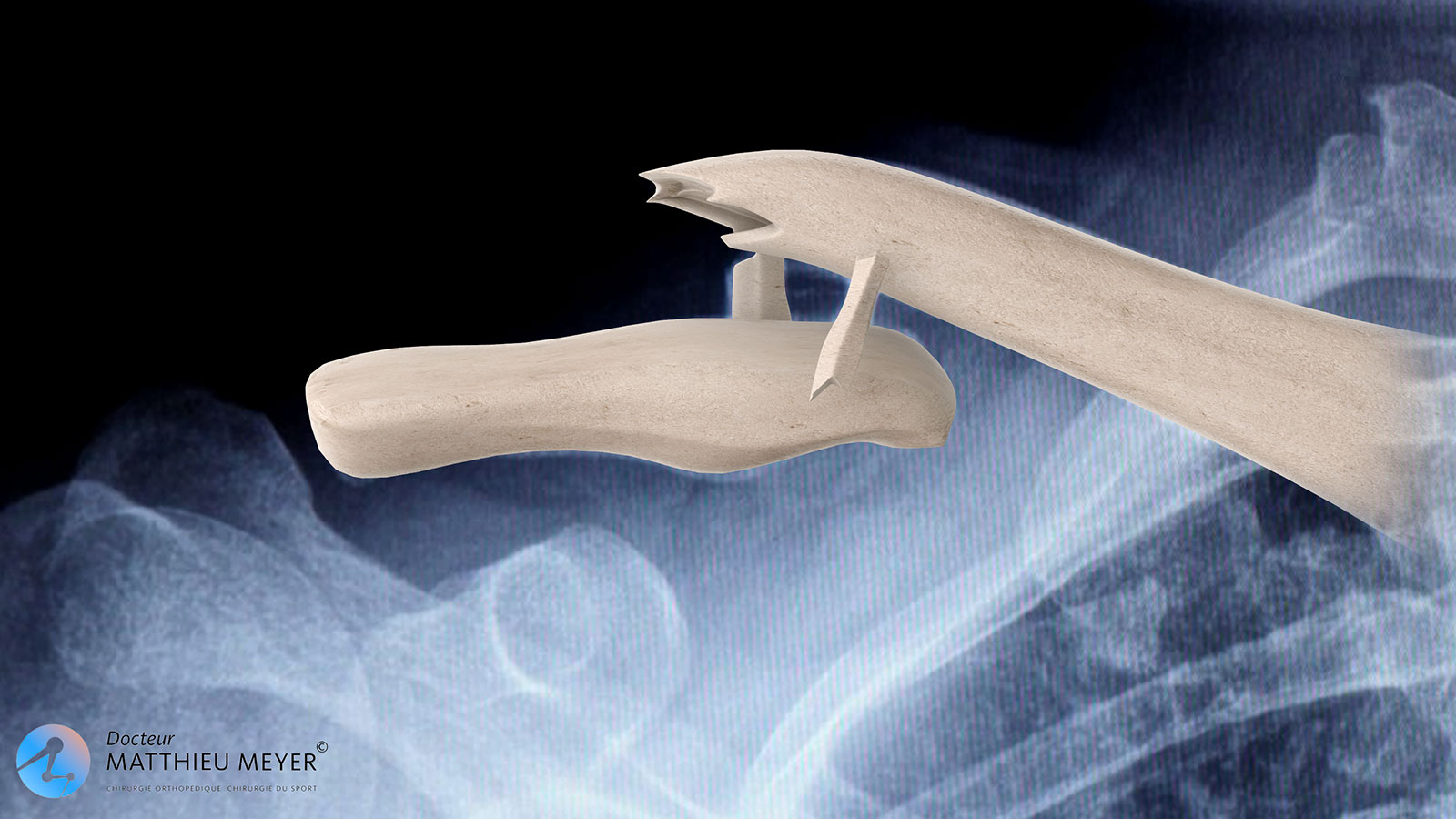
The clavicle is an s-shaped bone between the sternum and the scapula that plays an essential role in shoulder and arm movement. A fracture of the clavicle can occur during a fall on the lateral part of the shoulder and in 80% of cases involves the middle section.
For a long time, fractures of the clavicle were simply immobilised, even if the fracture was greatly displaced. The outcome of non-surgical treatment is often better in children and adolescents, whereas in adults healing of some fractures, especially multi-fragment displaced fractures, can be difficult or result in a poor functional outcome if the clavicle heals in a non anatomical position.
Understanding clavicle fractures
The number of fracture fragments and the displacement between these fragments will determine the choice of treatment.
The clavicle is surrounded by a membrane called the periosteum, which is thick and resistent in children and adolescents thus limiting the displacement of the fragments in the event of a fracture.
However, in adults, the periosteum is very thin and tears as a result of trauma and so does not restrict the displacement of the fragments, which is often considerable, especially with fractures of the middle third of the clavicle where the internal fragment is pulled upwards by the sternocleidomastoid muscle and the external fragment is pulled down by the deltoid muscle and the weight of the arm.
What examinations are necessary?
The imaging examinations must systematically include an x-ray of the clavicle. A CT-scan is often performed as well when surgical treatment is considered. These examinations determine the number of fracture fragments and their displacement.
In the case of neurological complications, an electromyogram can be requested to assess nerve damage. An angiography can also be requested if there is a vascular complication.
The various treatments available
Non-surgical or “orthopaedic” treatment
Orthopaedic treatment is based on immobilisation of which the duration depends on the age and type of fracture and can be between 3 and 6 weeks. There are two methods of immobilisation, which can sometimes be combined:
Immobilisation in a sling with the elbow against the body
This treatment aims to limit downward traction due to the weight of the arm. It is for stable fractures only slightly displaced and causes, when it is the dominant arm, functional impairment as the hand cannot be used.
Immobilisation with figure 8 braces
Figure 8 braces hold the shoulders back and are indicated for displaced or unstable fractures. However, the reduction of the fracture is not perfect if it is displaced. Less restrictive than slings, they are sometimes badly tolerated and if they are too tight can cause pressure sores or neurological compression of the brachial plexus.
Surgical treatment
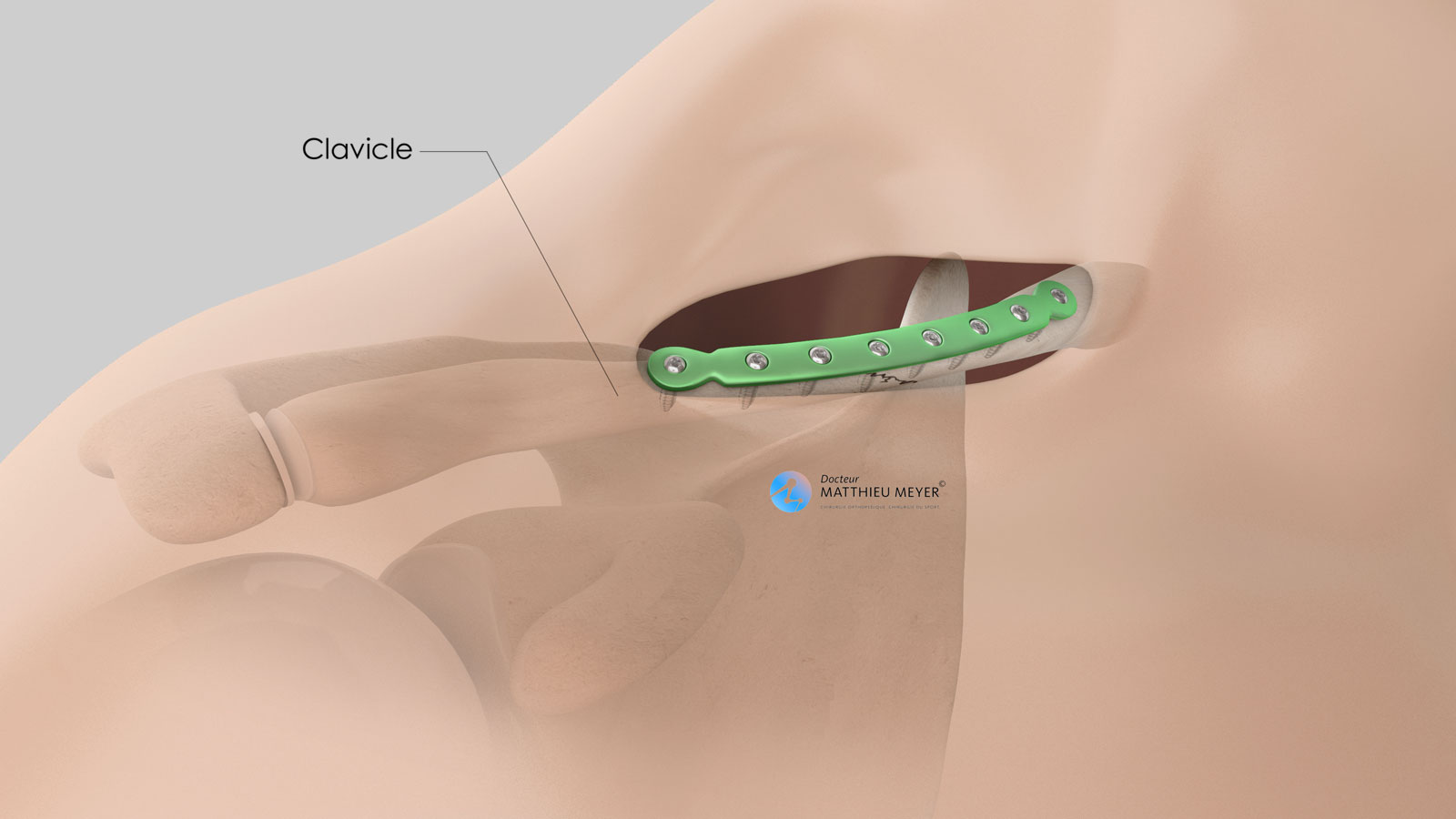
Surgical treatment involves reduction and osteosynthesis. The reduction consists in repositioning the different fragments to recover the clavicle’s original shape. Osteosynthesis ensures these fragments are held in place once they have been repositioned so the clavicle can heal in anatomical position. This osteosynthesis is most often achieved with a specific plate attached with screws that closely fits the shape of the clavicle.
Moreover, early rehabilitation is possible with surgical treatment, which is not the case with orthopaedic treatment.
Some fractures of the lateral quarter of the clavicle are similar to an acromioclavicular dislocation and are treated as such arthroscopically or with the insertion of an artificial ligament.
Progression and sequelae of non-surgical treatment
Non-surgical treatment of fractures for which the displacement is minimal is virtually systematic in children and young adolescents owing to the remodelling capacity of the bone as they are still growing.
In adults, orthopaedic treatment often results in the formation of a malunion, that is healing of the clavicle in a different shape to its original shape. These malunions are often well tolerated except in the case of significant shortening of the clavicle, which can affect arm range of motion is some positions. Sometimes, the malunion can be very voluminous, compressing neighbouring nerve and vascular structures and resulting in functional impairment of the upper limb.
It is also possible that the fracture of the clavicle does not heal. This is known as nonunion, which is more common in the case of orthopaedic treatment than surgical treatment. Nonunion is treated surgically and generally requires a bone autograft combined with the reduction and osteosynthesis of the fracture.
When is surgery necessary?
Surgical treatment with a plate fixed with screws has shown its superiority over orthopaedic treatment with a decrease in the risk of nonunion (no healing), better anatomical recovery, better functional outcome, and greater patient satisfaction including from an aesthetic point of view.
Surgical treatment is the only treatment that restores the physiological anatomy but there are more complications than with orthopaedic treatment, which is still very relevant in adults.
Even if there is no absolute consensus regarding the treatment of clavicle fractures, it is generally accepted that surgical treatment must be proposed in the following cases:
- Open fracture
- Fracture when one of the fragments may break the skin
- Fracture with nerve or vascular compression
- Multi-fragment fracture resulting in a higher risk of nonunion
- Displaced fracture with significant shortening of more than 15 mm
- Need to recover original anatomical shape for athletes or manual workers
The operation
Before the operation
Before the operation, a pre-anaesthesia consultation, and possibly a pre-operative assessment, is conducted to check the patient is physically apt to undergo the operation and minimise the risk of postoperative complications.
The operation
The operation takes place in an operating theatre in compliance with strict standards of cleanliness and safety. The patient is placed in beach chair position on an operating table. The operation lasts about 1 hour and is carried out under general anaesthesia, which is often combined with an interscalene nerve block. This additional anaesthetic maintains the shoulder and the arm numb for several hours and limits postoperative pain.
A horizontal incision, often between 5 and 7 centimetres, is made just below and parallel to the clavicle.
During the operation, the fracture is reduced and fixed with a plate and screws (osteosynthesis plate). A bone autograft with bone harvested from the pelvis is also carried out for old fractures that have not healed.
At the end of the procedure, a suction drain is often inserted in the incision to prevent the formation of hematoma.
After the operation
The shoulder is numbed with an interscalene block for 12 to 18 hours. Medication and ice also provide effective postoperative pain management.
The surgery can be performed as an outpatient procedure (leave hospital the day of the operation) or a short stay of 1 to 2 days. The patient can return home when discharged.
The shoulder is kept in an orthopaedic sling for 6 weeks. Gentle, passive rehabilitation begins early in the week following the operation to stop the shoulder from getting stiff. It is then intensified from the 4th week after the operation and is often completed in the 2nd month after the operation.
When the patient is discharged from the clinic, a consultation with follow-up x-rays is scheduled with the surgeon 4 to 6 weeks after the operation to check the fracture has not moved and the shoulder is healing well. A second check-up is generally recommended approximately 3 months after the operation.
The duration of medical leaves depends on the patient’s profession but generally varies between 4 and 6 weeks. It is longer for manual work.
Driving can be resumed 1 month after the operation.
Sports can be resumed using the shoulder operated on approximately 2 to 3 months after the operation depending on the progress made and the sport.
Risks linked to the operation
Unfortunately, zero risk does not exist in surgery. Any operation has its risks and limitations, which you must accept or not undergo the operation. However, if an operation is proposed, the surgeon and the anaesthetist consider that the expected benefits far outweigh the risk incurred.
Some risks, such as microbial infections of the surgical site, are common to all types of surgery. Fortunately, this complication is rare but when it occurs requires another operation and a course of antibiotics. Bruising can also appear around the surgical site. This is usually prevented or reduced with a suction drain inserted at the end of the operation and removed in the days following the operation. However, in the case of severe bleeding during or following the operation, another operation to stop the haemorrhage or a blood transfusion may be required.
Blood clots can form in the veins in the arm (thrombophlebitis) or lungs (pulmonary embolism). If the anaesthetist considers the risk high, you may be given a treatment to prevent this, which is rare.
In rare cases, the shoulder remains stiff, hot, and painful for several months after the operation. This complication, known as algodystrophy or Chronic Regional Pain Syndrome (CRPS), is unpredictable and sometimes takes a long time to heal.
Other rarer complications can also occur. Blood vessels (arteries, veins) can be accidentally damaged and require vascular surgery (bypass). Nerves can also be damaged accidentally during the operation with a risk of paralysis or loss of feeling in the limb operated on, which can be transitory or permanent.
Finally, the fracture may not heal and the plate can break over time and under the strain.
If you have any concerns about the operation, do not hesitate to talk to your surgeon or the anaesthetist and they will answer any questions you may have.
Does the osteosynthesis plate need to be removed?
The plate is not systematically removed and keeping it is not a problem. Its removal is however considered if the plate is perceived as bothersome in the long term, which is possible as it is located just under the skin.
Another operation is required to remove the plate and it is necessary to undergo a CT-scan to check the clavicle has healed perfectly.
In summary...
When is surgery necessary?
Severely displaced multi-fragment fracture / Manual worker / Athletic patient
Aim of the operation
Restore the anatomy of the clavicle and stabilise it to help it heal
Which anaesthesia?
General
Duration of hospitalisation
Outpatient or short stay (1 to 2 nights)
Postoperative immobilisation
Orthopaedic sling for 6 weeks with early mobilisation
Duration of rehabilitation
1 to 2 months
Duration of medical leave
4 to 6 weeks in the case of sedentary work, longer for manual work
Resumption of car driving
1 month after the operation
Resumption of sport
2 to 3 months after the operation
Make an appointment
please do not hesitate to contact us or make an appointment online via DoctoLib