In summary...
When is surgery necessasry?
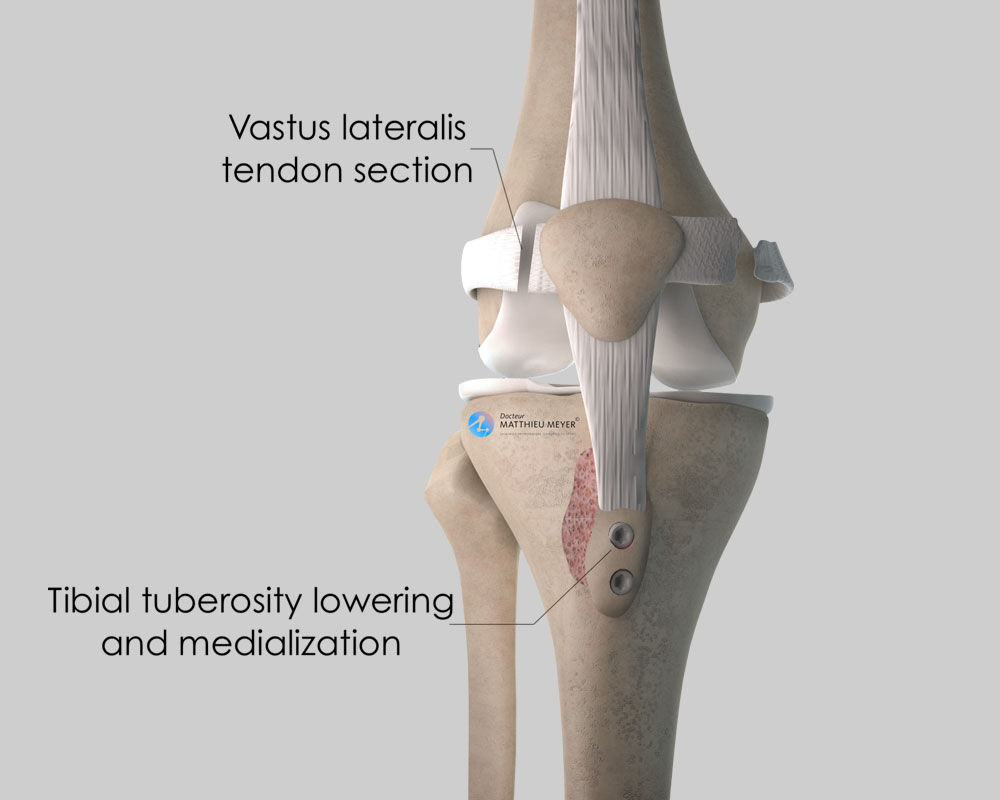
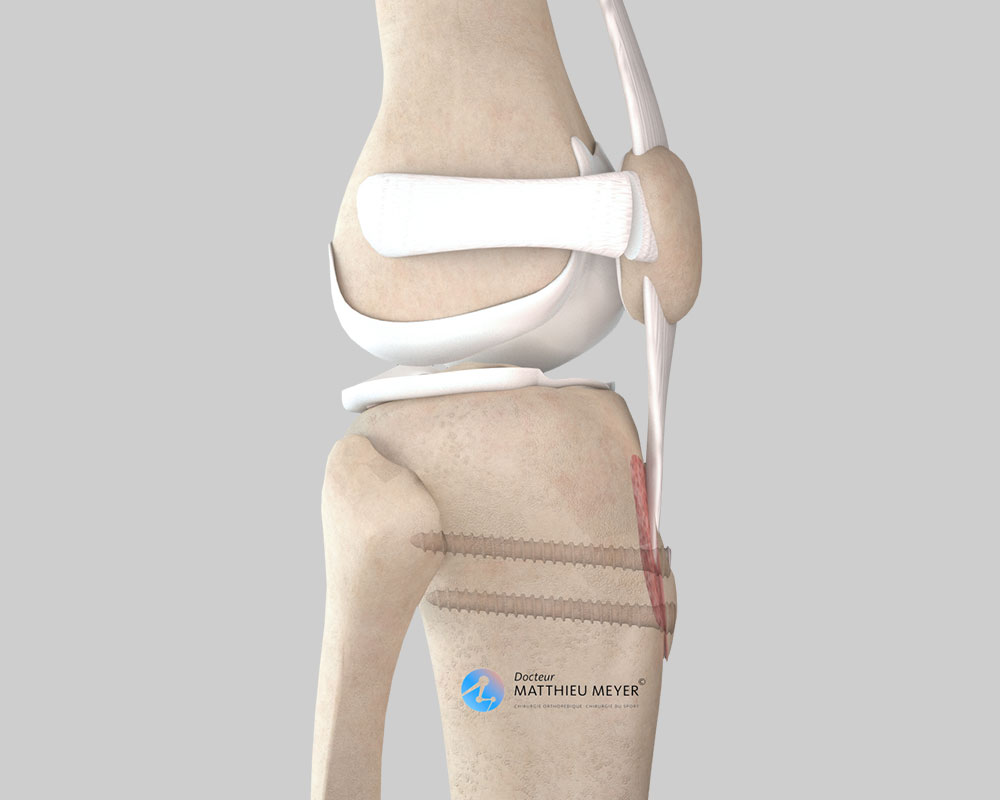
In the case of recurrent patellar dislocations, when the position of the ATT is too lateral and/or too high
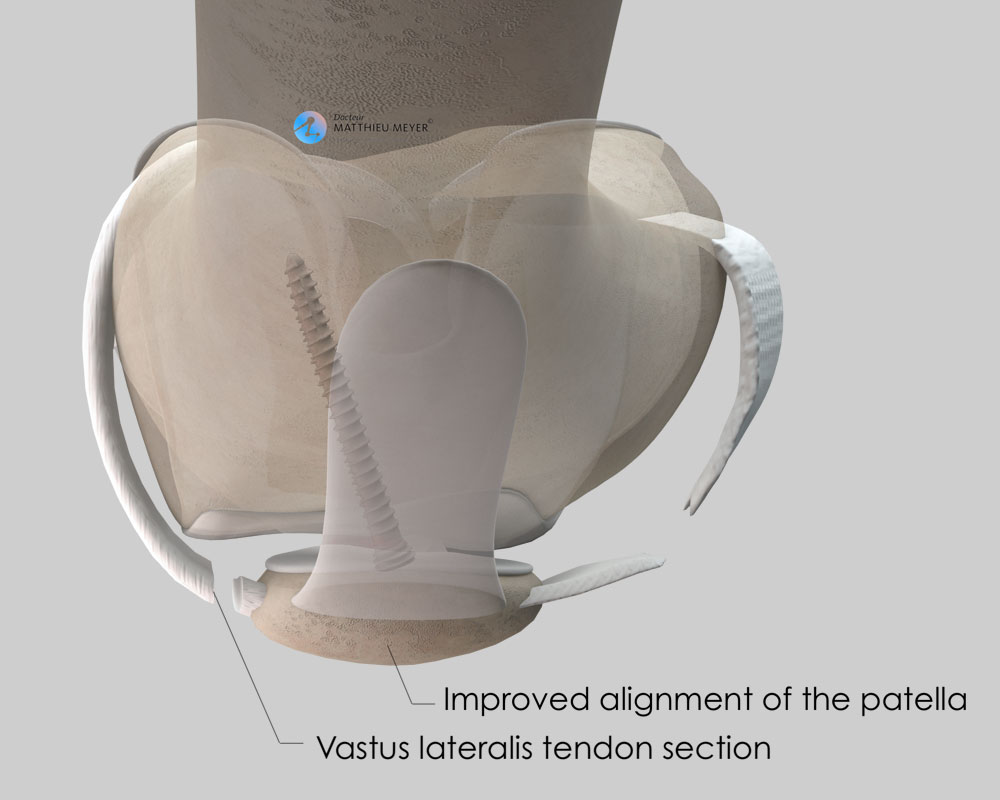
Aim of the operation
Stabilise the patella
Which anaesthesia?
General or regional (determined with the anaesthetist)
Duration of hospitalisation
Between 1 and 3 days
Resumption of weight-bearing
Immediately with a brace immobilising the knee
After the operation
Return home
Duration of rehabilitation
Generally 2 to 3 months
Duration of medical leave
6 to 8 weeks, longer for heavy work
Resumption of car driving
1½ months after the operation
Resumption of sport
4 months after the operation