Medical treatments, orthoses, and rehabilitation
In the days following the trauma, the knee is swollen due to the blood from the ligament tear making it difficult to bend the knee.
Walking is also difficult due to the sprain and quadriceps activation failure, which means the muscle cannot contract and no longer blocks the knee as it would normally.
The initial treatment must therefore act on all these symptoms.
The pain is treated with analgesics and anti-inflammatories. It is also recommended to put ice on the knee 4 to 6 times a day for the first few days following the trauma. When the knee is extremely taut and painful, the doctor can carry out an aspiration of the knee with a syringe to drain the bruise and thus relieve the pressure inside the joint.
A rigid brace (orthosis) will also be worn the aim of which is twofold: stop the knee giving way every time you put weight on it due to the quadriceps activation failure and help any torn lateral ligaments to heal at the same time as the anterior cruciate ligament.
Rehabilitation can begin early to recover joint range of motion and strengthen the quadriceps muscle.
→ Patients presenting an unstable knee
Anterior cruciate ligament rupture results in anterior knee instability. In some cases, the instability leads to a feeling of insecurity for the patient when putting weight on the knee; it feels as if it could give way. In other cases, this instability leads to the knee giving way, potentially resulting in a fall.
When the patient complains of instability, a ligamentoplasty (anterior cruciate ligament reconstruction) can be proposed.
Whether there is knee instability or not, a ligamentoplasty is proposed from the outset for some professions involving working at height (e.g. roofer), as the knee giving way could have dramatic consequences in the case of a fall.
→ Patients not presenting an unstable knee
In some cases, the knee remains stable, especially thanks to the menisci which have a dual role: ensuring knee stability and absorbing some of the strain to protect the knee from osteoarthritis. An anterior cruciate ligament tear puts the menisci under greater strain, increasing the risk of a meniscal tear. In young patients, this damage is linked to a risk of early knee osteoarthritis, which means anterior cruciate ligament reconstruction may be necessary in young patients to spare the menisci and indirectly prevent the onset of early knee osteoarthritis. In patients who do not complain about anything, this is called “preventive” surgery. In the latter case, it is necessary to weigh up the need for surgery, as this operation does not offer much hope for the patient in the short term but offers benefits in the medium and long term.
Consequently, in patients under 30 years with no knee instability, we tend to propose anterior cruciate ligament reconstruction. For patients between 30 and 40 years, we tend to operate when the knee is under a lot of strain (athletic patients doing pivoting sports: football, rugby, handball, judo, ski…).
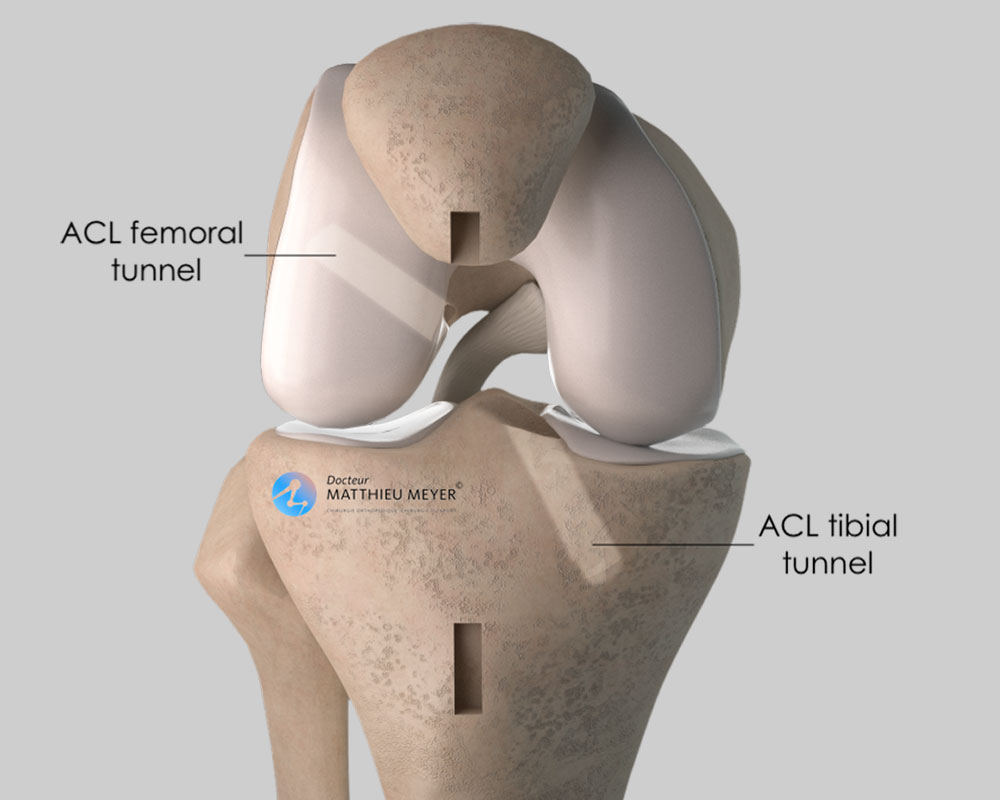
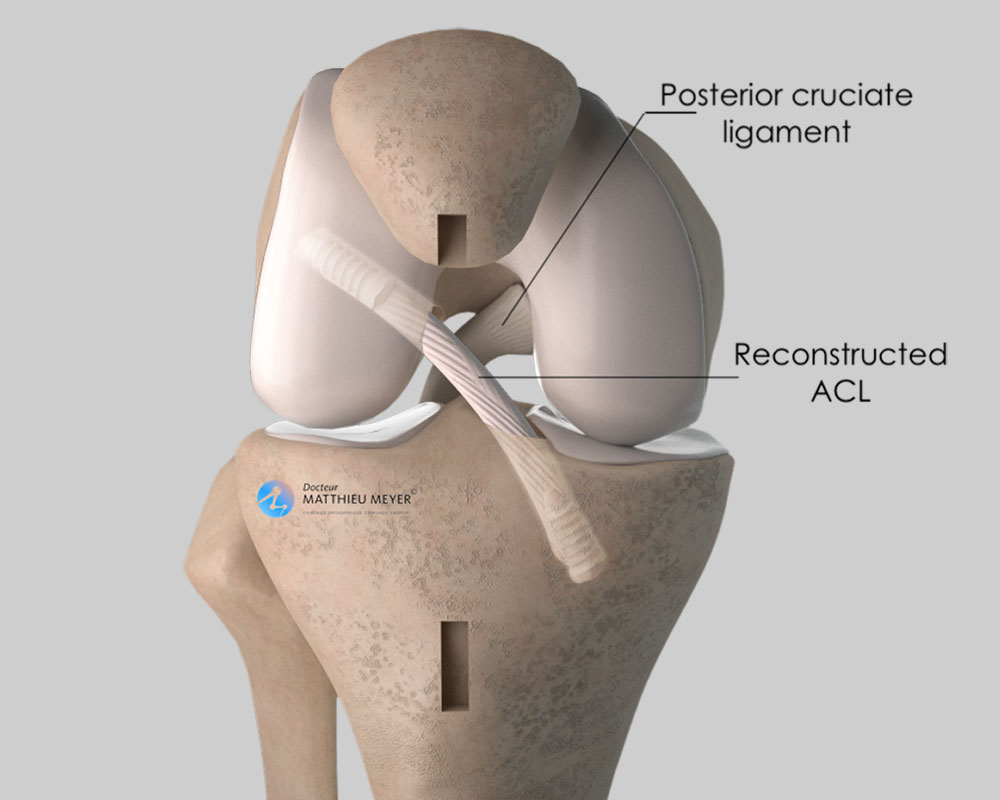
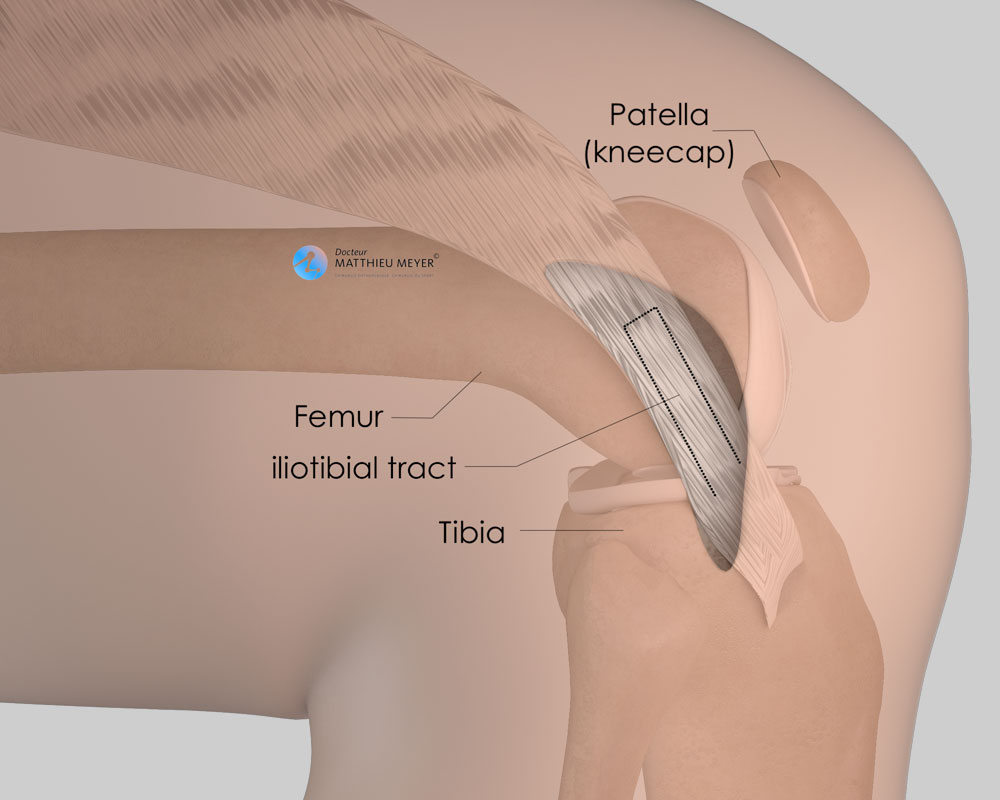
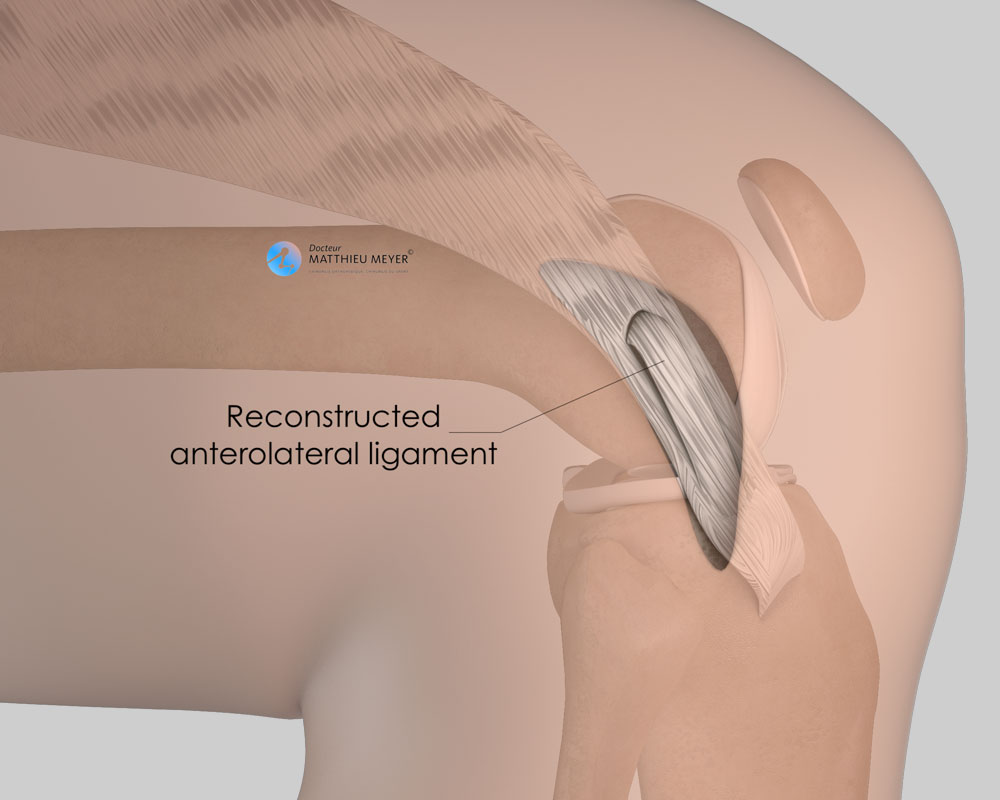
An anterior cruciate ligament ligamentoplasty consists in reconstructing the ligament.
The best results are achieved when the ligamentoplasty is performed on a knee that has recovered from the initial sprain following rehabilitation sessions to reduce the swelling and recover normal mobility. The surgery is, therefore, elective and is generally carried out several weeks after the initial trauma. However, the best results in terms of controlling knee laxity are obtained if the operation is performed in the first 6 months after the trauma.
More rarely, the initial sprain is combined with a bucket handle meniscal tear causing the knee to lock during bending. In these circumstances, rehabilitation of the knee is not possible and the procedure must be performed rapidly to treat the meniscal tear at the same time as the anterior cruciate ligament ligamentoplasty and thus unlock the knee.
In the absence of surgery, there may be numerous consequences. The knee can become very unstable and it will be impossible to do some sports. Furthermore, the menisci may tear causing pain and even clicking of the knee. Ultimately, in the case of significant meniscal damage, osteoarthritis can develop.